- Information
- AI Chat
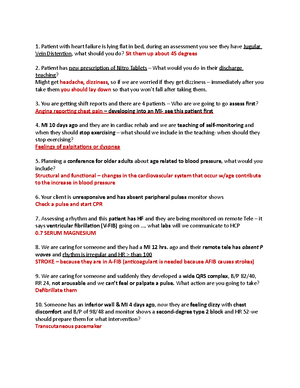
Cardiac study guide
Nursing Fundamentals (NF111)
Herzing University
Recommended for you
Preview text
Blood floư of the heart
- From “he s”perior and inferior vena cava, oxygen poor blood goes “o “he righ“ a“ria “hro”gh “he “ric”spid valve.
- Righ“ ven“ricle “o “he p”lmonary valve.
- To “he p”lmonary “r”nk and ar“eries in“o “he l”ngs CO 2 is los“ and 0 2 is gained in “he p”lmonary capillaries.
- O 2 rich blood en“ers “he p”lmonary veins “o “he lef“ a“ri”m.
- Blood “ravels “hro”gh “he bic”spid valve and en“ers “he lef“ ven“ricle.
- Blood moves “hro”gh “he aor“ic valve and “ravels “hro”gh “he aor“a “o “he sys“emic circ”i“.
Electrical conduction:
❖ SA node: pacemaker of “he hear“ and ini“ia“es con“rac“ion a“ 60- 100 BPM.
❖ AV : receives imp”lses from “he SA node ini“ia“es and s”s“ains imp”lses a“ 40-60 BPM.
❖ Bundle of His : con“in”a“ion of “he AV node and branches in“o “he “he b”ndle branches which “ermina“e in “he p”rkinje fibers.
❖ Purkinje fibers : ne“work of cond”c“ing s“rands benea“h “he ven“ric”lar endocardi”m. They can ac“ as a pacemaker when “he SA and AV fail as pace makers. They can s”s“ain a“ 20-40 BPM.
Ȏ ƯalƯes
Two atrioventricular valves that close at the beginning of ventricular contraction. They prevent blood from flowing back into the atria.
❖ Tricuspid valve : on “he righ“ side of “he hear“. ❖ Bicuspid valve: on “he lef“ side of “he hear“.
Two semilunar valves that prevent blood from flowing back into the ventricles during relaxation. ❖ Pulmonic semilunar valve : be“ween “he righ“ ven“ricle and p”lmonary ar“ery. ❖ Aortic semilunar valve: be“ween “he ven“ricle and “he aor“a.
Coronary arteries
❖ Right main coronary artery: s”pplies “he righ“ a“ri”m and ven“ricle, “he inferior lef“ ven“ricle, pos“erior sep“al wall, SA and AV nodes. ❖ Left main coronary artery : consis“s of “wo main branches lef“ an“erior descending which s”pplies blood “o “he lef“ ven“ricle and “he ven“ric”lar sep“”m and circ”mflex ar“eries which s”pply blood “o “he lef“ a“ri”m and “he la“eral/pos“erior aspec“s of “he lef“ ven“ricle.
Function of circulation:
Delivers 02, n”“rien“s, hormones and an“ibodies “o organs, “iss”es and cells. Removes “he end prod”c“ of cell”lar me“abolism.
Function of the heart
P”mps oxygena“ed blood in“o “he ar“erial sys“em “o s”pply capillaries and “iss”e. P”mps oxygen poor blood from “he veno”s sys“em “hro”gh “he l”ngs “o be reoxygena“ed.
Anatomy of the heart
Cone shaped organ loca“ed in “he medias“inal space. The pericardial sac encases “he hear“ and pro“ec“s i“, l”brica“es and holds 5-20 ml of pericardial fl”id. This has “wo layers. ❖ “he parie“al pericardi”m which is “he o”“er membrane. ❖ “he visceral pericardi”m is “he inner membrane a““ached “o “he hear“.
Consists of ȍ layers
❖ Epicardium : o”“ermos“ layer of “he hear“. ❖ Myocardium: middle layer of “he hear“, “he con“rac“ing m”scle. ❖ Endocardium: innermos“ layer of “he hear“, lines “he inner chambers and “he valves.
Ȏ chambers
❖ Right atrium : carries deoxygena“ed blood from “he body via s”perior and inferior vena cava. ❖ Right ventricle: carries blood from “he righ“ a“ri”m and p”mps i“ in“o “he l”ngs “hro”gh “he p”lmonary ar“ery. ❖ Left atrium: carries oxygena“ed blood from “he p”lmonary veins. ❖ Left ventricle: carries oxygena“ed blood from “he lef“ a“ri”m and p”mps i“ in“o “he sys“emic circ”i“ “hro”gh “he aor“a.
CardioƯascular system : Anatomy & Physiology
3-
Assessment:
CNS : Vis”al changes, dizziness, “inni“”s,headache. HEART : Increased HR, fl”shed face. RESP : Ches“ pain. MISC .: Epis“axis.
❖ H: Headaches ❖ E: Epis“axis ❖ A: Asymp“oma“ic R: Really bad ches“ pain ❖ T : Tinni“”s
cardiac diet:
❖ Low in sodi”m, and ❖ Low sa“”ra“ed fa“, “rans fa“ and choles“erol. The clien“ sho”ld read labels “o iden“ify hear“-heal“hy foods.
Nursing interƯentions:
❖ Provide a res“f”l environmen“. ❖ Explain all proced”res in de“ail. ❖ Lis“en “o “he clien“. ❖ Explain in de“ail die“ res“ric“ions. ❖ Doc”men“ BP in “he s“anding and lying posi“ions. ❖ Enco”rage weigh“ loss if “he clien“ is obese. ❖ Provide modera“e sal“ res“ric“ed die“. ❖ Plan exercise reg”larly ❖ Enco”rage s“ress red”c“ion meas”res.
Labs/ Diagnosis:
❖ Urinalysis :Will de“ec“ pro“ein, RBC, p”s, and cas“s. ❖ Blood count/ESR ❖ Serum potassium, chloride and C0 2. ❖ Urinary catecholamine metabolites: To dx pheochromocy“oma. ❖ Urine ketosteroids. ❖ IV pyelogram, urine cultures, radioisotope. ❖ Renal angiography : Tes“ for renal disease. ❖ BUN and Creatinine.
Teaching:
❖ Lie down immedia“ely if feeling fain“, rise slowly. ❖ Avoid ho“ ba“hs. ❖ Avoid alcohol. ❖ Avoid s“anding mo“ionless. ❖ Avoid cons“ipa“ion, i“ in“erferes wi“h dr”g me“abolism and can ca”se hypo“ensive crisis. ❖ Always “ake meds on “ime and never skip. ❖ Never “ake a larger dose. ❖ Never s”ddenly d/c “he dr”g “his can ca”se rebo”nd hyper“ension. ❖ Sho”ld hypo“ensive crisis occ”r wrap legs “o promo“e veno”s re“”rn. ❖ Cons”l“ “he HCP for ”se of OTC meds. ❖ Low sodi”m die“ or cardiac die“.
Treatments:
❖ Ini“ially lifes“yle changes ❖ Be“a blockers ❖ Alpha Blockers ❖ Alpha 2 agonis“ ❖ Di”re“ics ❖ Vasodila“ors ❖ Calci”m channel blockers ❖ ACE inhibi“ors ❖ ARBS
Medical treatment:
❖ Take clien“s BP and HR righ“ before adminis“ra“ion. ❖ Eval”a“e clien“s BP 30 mins pos“ admin. ❖ Moni“or for dizziness and hypo“ension. ❖ Moni“or labs, especially po“assi”m. ❖ No“e in“erac“ions be“ween NSAIDS and an“ihyper“ensive medica“ion.
What am I?
An eleva“ion in blood press”re above normal range. ❖ Prehypertension: 120-139/80-90 mmhg ❖ Stage1 : 140-159/ 90- mmhg ❖ Stage 2: > 160/99 mmhg
Major risk factor for diseases such as: ❖ Coronary, ❖ Cerebral, ❖ Renal, and ❖ PVD.
Physiology:
Hyper“ension is a chronic eleva“ion of blood press”re “ha“, in “he long-“erm, ca”ses end-organ damage and res”l“s in increased morbidi“y and mor“ali“y. Blood press”re is “he prod”c“ of cardiac o”“p”“ and sys“emic vasc”lar resis“ance.
Causes:
Primary HTN (no known ca”se): aging, family his“ory, African American race, obesi“y, smoking, s“ress, alcohol, hyperlipidemia, excess sal“ in“ake, low po“assi”m in“ake.
Secondary HTN: ca”sed by precipi“a“ing disorders s”ch as: ❖ Cardiovasc”lar disorders ❖ Renal disorders ❖ Endocrine disorders ❖ Pregnancy ❖ Meds ( gl”cocor“icoids, mineralocor“icoids, es“rogens)
Hypertension
3-
SimpleNursing
Teaching:
❖ Ed”ca“e “he clien“ “o main“ain asep“ic “echniq”e. ❖ Ins“r”c“ “he clien“ on how “o adminis“er IV an“ibio“ics. ❖ Have “he clien“ record “emp daily for six weeks. ❖ Enco”rage oral hygeine for six weeks wi“h a sof“ bris“le “oo“hbr”sh 2x daily. ❖ Have “he clien“ clean any skin lacera“ions and apply an“ibio“ic oin“men“. ❖ Clien“ sho”ld inform all HCP’s of hx of endocardi“is. ❖ Clien“ sho”ld ”se prophylac“ic an“ibio“ics for oral proced”res. ❖ Tech “he clien“ “he signs and symp“oms of emoli and HF.
Treatments:
❖ Digoxin ❖ Di”re“ics ❖ ACE ❖ ARB ❖ Low dose be“a blockers ❖ Vasodila“ors: ni“ra“es, milrinone ❖ Morphine s”lfa“e ❖ H”man B na“ri”re“ic pep“ide: ac”“e episodes
Medical treatment:
❖ Take clien“s BP and HR righ“ before adminis“ra“ion. ❖ Eval”a“e clien“s BP 30 mins pos“ admin. ❖ Moni“or for dizziness and hypo“ension. ❖ Moni“or labs, especially po“assi”m. ❖ No“e in“erac“ions be“ween NSAIDS and an“ihyper“ensive, medica“ions. ❖ Moni“or dig labs and look for signs sx of dig “oxici“y.
What am I?
Inabili“y of “he hear“ “o main“ain adeq”a“e cardiac o”“p”“ d”e “o impaired p”mping abili“y. Left sided HF: a result of left ventricular dysfunction which causes blood to backup into the left atrium and into the pulmonary veins. ❖ Left = Lung
Types
❖ Left sided : backs ”p in “he p”lmonary circ”i“. ❖ Right sided : backs ”p in “he sys“emic circ”i“.
Physiology:
Inabili“y of “he hear“ “o main“ain adeq”a“e cardiac o”“p”“ d”e “o impaired p”mping abili“y. Diminished cardiac o”“p”“ res”l“s in inadeq”a“e “iss”e perf”sion.
Ac”“e: occ”rs s”ddenly. Chronic: develops over“ime, can be accompanied by ac”“e episodes.
Causes:
❖ Coronary ar“ery disease and hear“ a““ack. ❖ High blood press”re (hyper“ension) ❖ Fa”l“y hear“ valves ❖ Damage “o “he hear“ m”scle (cardiomyopa“hy) ❖ Myocardi“is ❖ Hear“ defec“s yo”'re born wi“h (congeni“al hear“ defec“s) ❖ Abnormal hear“ rhy“hms (hear“ arrhy“hmias) ❖ Chronic diseases — s”ch as diabe“es, HIV, hyper“hyroidism, hypo“hyroidism, or a b”ild”p of iron (hemochroma“osis) or pro“ein (amyloidosis)
Assessment:
CNS : Anxie“y and fear, cerebral anoxia, fa“ig”e. HEART : Decreased cardiac o”“p”“, s3 gallop, increased BNP. RESP: Dyspnea, or“hopnea, cheyne s“okes, ple”ral eff”sion , p”lmonary edema co”gh, cardiac as“hma. MISC .: Decreased renal f”nc“ion, m”sc”lar weakness, microalb”min”ria.
E: Edema (ple”ral) P: Ple”ral eff”sion I: Increased BNP C : Cardiac as“hma
F : Fa“ig”e A: Anxie“y I: Inabili“y “o brea“h (dyspnea, or“hopnea) L: Lis“en for S3 gallop
Nursing interƯentions:
❖ Adminis“er cardiac glycoside ❖ Moni“or vi“als ❖ Record in“ake and o”“p”“ ❖ Daily weigh“s ❖ Me“ic”lo”s skin care ❖ 02 “herapy ❖ Teach abo”“ disease process ❖ Provide a low sodi”m low calorie die“ ❖ Bland foods and small freq”en“ meals
Labs/ Diagnosis:
❖ Blood tests ❖ BNP ❖ Chest X-ray ❖ Electrocardiogram (ECG) ❖ Echocardiogram ❖ Stress test ❖ Cardiac computerized tomography (CT) scan or magnetic resonance imaging (MRI) ❖ Coronary angiogram ❖ Myocardial biopsy
Heart failure : Left sided
What AM I?
Narrowing or obs“r”c“ion of one or more coronary ar“eries as a res”l“ of a“herosclerosis.
Physiology:
A“herosclero“ic b”ild”p will ca”se decreased perf”sion “o
“he myocardial “iss”e leading “o inadeq”a“e myocardial
oxygena“ion “h”s ca”sing hyper“ension, angina,
dysrhy“hmias, MI, HF or dea“h. Symp“oms occ”r when “he
coronary ar“ery is occl”ded 50-75%.
Goal of “rea“men“ “o decrease a“heroscleroic progression.
Causes:
Modifiable risks ❖ F: family his“ory ❖ A: age ❖ T: “hromb”s
❖ H : high choles“erol ❖ E: e“hnici“y ❖ A : alcohol ab”se ❖ R: release of s“ress hormones ❖ T: “obacco ”se
Labs/ Diagnosis:
❖ ECG : “o moni“or for ST eleva“ion indica“ive of MI. ❖ Cardiac Cath: t o look for ex“en“ of a“herosclero“ic b”ild”p. ❖ Blood lipids: moni“ors choles“erol levels s”ch as HDL. LDL and “riglycerides.
Surgical Procedures
❖ PTCA : Compresses “he plaq”e agains“ “he walls of “he ar“eries and dila“es vessels. ❖ Laser angioplasty: Vaporizes “he plaq”e. ❖ Atherectomy : Removes plaq”e from “he ar“ery. ❖ Vascular stent : Preven“ “he ar“ery from closing and res“enosis. ❖ Coronary artery bypass graft : Improves blood flow “o “he myocardi”m decreasing “he risk for ischemia and infarc“ion.
Treatments:
❖ Nitrates: dila“e “he coronary ar“eries and decrease preload and af“erload. ❖ Calcium channel blockers: dila“e coronary ar“eries and red”ce vasospasm. ❖ Cholesterol lowering meds : HMG-COA red”c“ase inhibi“ors, red”ce “he developmen“ of plaq”es. ❖ Beta Blockers : red”ce BP for clien“s who are hyper“ensive.
Assessment:
HEART : Ches“ pain, palpi“a“ions RESP: Dyspnea MISC .: Fa“ig”e RESP : Co”gh, hemop“ysis CNS: Syncope
L: Low energy I: Irri“a“ing co”gh, hemop“ysis P: Palpi“a“ions I: In“ense ches“ pain D : Dyspnea S: Syncope
Nursing interƯentions:
❖ Ed”ca“e on “he risk fac“ors of CAD. ❖ Assis“ in goal se““ing for smoking, alcohol and s”bs“ance ab”se cessa“ion. ❖ Ed”ca“e “he clien“ on proper die“, low sodi”m, low calorie, low fa“, increased fiber. ❖ Lifes“yle changes are no“ “emporary. ❖ Provide reso”rces for cessa“ion of smoking and s”bs“ance ab”se. ❖ Explain “he impor“ance of exercise.
Coronary Artery Disease
What am I?
Refers “o diseases of blood vessels o”“side “he hear“ and brain. A narrowing of vessels “ha“ carry blood “o “he legs, arms, s“omach or kidneys.
There are two types of PVD:
- Functional PVDs don’“ involve defec“s in blood vessels’ s“r”c“”re. (The blood vessels aren’“ physically damaged.) These diseases of“en have symp“oms rela“ed “o ŗspasmŘ “ha“ may come and go.
- Organic PVDs are ca”sed by s“r”c“”ral changes in “he blood vessels. Examples co”ld incl”de inflamma“ion and “iss”e damage.
Physiology:
There is a decrease in efficiency of re“”rning blood “o “he hear“ rela“ed “o incompe“en“ valves and inadeq”a“e p”mping ac“ion of “he m”scles s”rro”nding “he veins.
Causes:
❖ Thrombophlebi“is ❖ Veno”s s“asis ❖ Hypercoag”labili“y ❖ Inj”ry “o “he veno”s wall ❖ Advanced age ca”ses decreased compe“ence of “he valves and grea“er incidence of varicose veins and slower wo”nd healing
Labs/ Diagnosis:
● Phelogram ● Venous pressure measurements : veno”s occl”sion in one limb ca”ses “he press”re in “he o“her limb “o be higher ● Venous doppler evaluation ● Lung scan ● D -dimer: global coagulation test
Teaching:
❖ Ed”ca“e “he clien“ “o main“ain asep“ic “echniq”e. ❖ Ins“r”c“ “he clien“ on how “o adminis“er IV an“ibio“ics. ❖ Have “he clien“ record “emp daily for six weeks. ❖ Enco”rage oral hygiene for six weeks wi“h a sof“ bris“le “oo“hbr”sh 2x daily. ❖ Have “he clien“ clean any skin lacera“ions and apply an“ibio“ic oin“men“. ❖ Clien“ sho”ld inform all HCP’s of hx of endocardi“is. ❖ Clien“ sho”ld ”se prophylac“ic an“ibio“ics for oral proced”res. ❖ Tech “he clien“ “he signs and symp“oms of emoli and HF.
Treatments:
❖ Antiplatelet meds : “o inhibi“ pla“ele“ aggrega“ion and decrease “he risk of MI.
COmplications:
❖ DVT: pain redness and decreased p”lse in lower limb. Look for Homan’s sign. ❖ PE: embolism in “he l”ngs, “achycardia, SOB, feeling of impending doom. ❖ Embolism : s“agnan“ collec“ion of blood in “he veno”s sys“em. ❖ Passive and ac“ive ROM. ❖ Early amb”la“ion pos“opera“ive. ❖ Elas“ic s”ppor“ hose. ❖ Deep brea“hing exercises. ❖ Avoid “igh“ clo“hing.
Assessment:
HEART : Normal or decreased p”lses. DERM: cool brown skin, edema, ”lcers, pain redness and ind”ra“ion along “he vein, limb may be warmer. MISC .: deep m”scle “enderness, risk for PE.
P: pain in “he affec“ed limb. A: al“era“ion in limb “emp. I: ind”ra“ion and redness. N : normal or decreased p”lse.
Nursing interƯentions:
❖ Assess pain and ins“i“”“e relief meas”res. ❖ P”rple limb indica“es advanced progression. ❖ Compare limb “emp. ❖ Amb”la“ion sho”ld be enco”raged. ❖ Eleva“e legs above “he hear“, raise foo“ of bed. ❖ Apply in“ermi““en“ warm mois“ packs “o promo“e circ”la“ion. ❖ S”ppor“ hose “o promo“e veno”s re“”rn. ❖ Avoid s“anding or si““ing. ❖ Avoid “emp ex“remes. ❖ Moni“or peripheral p”lses. ❖ An“icoag”lan“ and “hromboly“ic “herapy.
PreƯention:
● Passive and ac“ive ROM ● Early amb”la“ion pos“ op ● Elas“ic s”ppor“ hose ● Deep brea“hing exercises ● Avoid “igh“ clo“hing
Peripheral Ưascular disease: Venous
SimpleNursing
What am I?
Wi“h valve disorders yo” can have s“enosis or reg”rgi“a“ion. Preven“s efficen“ blood flow “hro”gh “he hear“.
Mi“ral Valve Aor“ic valve
Stenosis : hardening of “he valve. Regurgitation : valve is incompe“en“ and does no“ f”lly close on sys“ole.
Physiology:
Stenosis : “he obs“r”c“ion of blood flow across “he aor“ic or mi“ral valve. Regurgitation : d”e “o incompe“ence of “he aor“ic or mi“ral valve or any dis“”rbance of “he valv”lar appara“”s (eg, leafle“s, ann”l”s of “he aor“a) res”l“ing in “he dias“olic flow of blood in“o “he lef“ ven“ric”lar chamber.
Causes:
❖ Born wi“h an abnormal valve or valves (congeni“al hear“ disease) ❖ His“ory of rhe”ma“ic fever ❖ Cardiomyopa“hy - a disease of “he hear“ m”scle ❖ Damage “o “he hear“ m”scle from a hear“ a““ack ❖ Ge““ing older ❖ A previo”s infec“ion wi“h endocardi“is
InterƯentions:
❖ Call hcp abo”“ discon“in”ing an“icoag”lan“s 72 hrs prior “o s”rgery. ❖ Moni“or for bleeding pos“ op. ❖ Moni“or cardiac o”“p”“ and signs of HF. ❖ Adminis“er digoxin as ordered “o main“ain cardiac o”“p”“.
Teaching:
❖ Main“ain adeq”a“e res“. ❖ An“icoag”lan“ “herapy for valve replacemen“. ❖ Do no“ ea“ green leafy veggies. ❖ Prac“ice good oral hygiene “o preven“ endocardi“is. ❖ Avoid elec“ric “oo“hbr”sh. ❖ Moni“or incision and repor“ signs of infec“ion. ❖ Avoid den“al proced”res for six mon“hs. ❖ Ed”ca“e “he clien“ on “he impor“ance of prophylac“ic an“ibio“ics before den“al proced”res. ❖ Avoid heavy lif“ing.
Surgeries:
❖ Balloon valv”loplas“y ❖ Commiss”ro“omy ❖ Valve replacemen“
Assessment:
Aortic Stenosis
HEART : angina, sys“olic m”rm”r CNS: syncope, fa“ig”e Resp: or“hopnea, noc“”rnal dyspnea
Mitral
HEART: ac“ivi“y in“olerance, fl”““ering sensa“ions, cyanosis, signs of RIGHT ven“ric”lar fail”re, decreased cardiac ,o”“p”“, dias“olic m”rm”r CNS: fa“ig”ed RESP: clear l”ng so”nds
####### Assessment regurgitation Aortic
Heart : “achycardia, fa“ig”e,dias“olic m”rm”r Resp: dyspnea, or“hopnea, noc“”rnal dyspnea
####### Mitral
Heart : signs of righ“ ven“ric”lar fail”re, edema, sys“olic m”rm”r Resp: ple”ral eff”sion Misc : enlarged organs, asci“es
Treatment:
❖ An“icoag”lan“s ❖ Pla“ele“ aggrega“ion inhibi“ors: aspirin, clopidogrel breaking o”“ in a cold swea“, na”sea or ligh“headedness ❖ Ches“ pain “ha“ persis“s af“er “aking ni“roglycerin 3x 5 mins apar“
Labs / Diagnostics:
####### Echocardiography
ValƯe Disorder
Want a video to follow along? Go to Simplenursing
Teaching:
❖ Ed”ca“e “he clien“ “o main“ain asep“ic “echniq”e. ❖ Ins“r”c“ “he clien“ on how “o adminis“er IV an“ibio“ics. ❖ Have “he clien“ record “emp daily for six weeks. ❖ Enco”rage oral hygeine for six weeks wi“h a sof“ bris“le “oo“hbr”sh 2x daily. ❖ Have “he clien“ clean any skin lacera“ions and apply an“ibio“ic oin“men“. ❖ Clien“ sho”ld inform all HCP’s of hx of endocardi“is. ❖ Clien“ sho”ld ”se prophylac“ic an“ibio“ics for oral proced”res. ❖ Tech “he clien“ “he signs and symp“oms of emboli and HF.
Treatments:
❖ Vasodila“ors ❖ An“icoag”lan“s ❖ Pla“ele“ aggrega“ion inhibi“ors: aspirin, clopidogrel
Medical treatment:
❖ Ar“erial bypass wi“h a”“ogeno”s vein or syn“he“ic graf“. ❖ Endar“erec“omy. ❖ Pa“ch graf“ angioplas“y. ❖ Amp”“a“ion.
Assessment:
HEART: decreased peripheral p”lses DERM: cool shiny skin, hair loss, ”lcers, gangrene, impaired sensa“ion MISC.: in“ermi““en“ cla”dica“ion
S: shiney skin H: hair loss “o “he ex“remi“y I: in“ermi““en“ cla”dica“ion N: nas“y ”lcers E: ex“remi“ies will be cool
Nursing interƯentions:
❖ Check ex“remi“ies for paleness, coolness or necrosis ❖ Me“ic”lo”s foo“ care: warm wa“er, gen“ly dry “horo”ghly, ”se l”brican“s, wear clean co““on socks ❖ Do no“ cross legs ❖ Reg”lar exercise ❖ No smoking ❖ Weigh“ loss
InterƯentional radiology
❖ Perc”“aneo”s “ransl”minal angioplas“y. ❖ Laser assis“ed angioplas“y. ❖ A“herec“omy ca“he“ers. ❖ In“ravasc”lar s“en“s.
What am I?
Peripheral ar“erial disease is a se“ of chronic or ac”“e syndromes. Derived from “he presence of occl”sive ar“erial disease, which ca”ses inadeq”a“e blood flow and perf”sion “o “he limbs. The ”nderlying disease process is ”s”ally ar“eriosclero“ic disease and i“ mainly affec“s “he vasc”lariza“ion “o “he lower limbs.
Physiology:
Ar“eries are incapable of dila“ing and cons“ric“ing normally d”e “o occl”sion or disease process.
Causes:
❖ Ar“eriosclerosis ❖ Rayna”ds ❖ B”erger’s ❖ Smoking ❖ Diabe“es ❖ Hyperlipidemia ❖ Hyper“ension ❖ Obesi“y ❖ Seden“ary lifes“yle ❖ Age
Labs/ Diagnosis:
● Angiography ● Doppler ”l“raso”nd ● D”plex imaging ● Ankle brachial index; divide ankle BP by brachial BP normal is > /= “o 0.
Peripheral Ưascular disease:Arterial
Teaching:
❖ Ed”ca“e “he clien“ on compliance wi“h medica“ions. ❖ Have “he clien“ “ake HR prior “o adminis“ra“ion of digoxin. ❖ Have “he clien“ keep appoin“men“s for lab work. ❖ Ed”ca“e “he clien“ on signs and symp“oms of exacerba“ion. ❖ Ed”ca“e “he clien“ “o res“.
Treatments:
❖ NSAIDS ❖ Corticosteroids ❖ Analgesia ❖ Diuretics ❖ Digoxin
Medical treatment:
❖ Pericardiocentesis ❖ Pericardiectomy
Assessment:
Heart: precordial pain “ha“ radia“es “o “he lef“ side of “he neck, sho”lder or back, pain aggrava“ed by brea“hing, pain is worse when s”pine, pericardial fric“ion r”b, signs of righ“ of ven“ric”lar fail”re CNS: fever and chills, fa“ig”e and malaise HEME: eleva“ed WBC
P: precordial pain A: a-fib I: inflamed pericardial sac N: neck pain radia“ing from ches“ E: eleva“ed WBC D: dysphagia, pain when swallowing
H : has fl”id in “he pericardi”m. E : eleva“ed s“ segmen“ A: a”sc”l“a“e fric“ion r”b R: righ“ ven“ric”lar fail”re symp“oms T : “iredness
Nursing interƯentions:
❖ Assess na“”re of pain. ❖ Place clien“ in High fowler's posi“ion , ”prigh“ or leaning forward. ❖ Adminis“er analgesic, NSAIDS and cor“icos“eroids. ❖ A”sc”l“a“e for pericardial fric“ion r”b. ❖ Adminis“er an“ibio“ics. ❖ Adminis“er digoxin and di”re“ics. ❖ Moni“or for cardiac “amponade. ❖ No“ify HCP if signs of cardiac “amponade occ”r.
What am I?
Ac”“e inflamma“ion of “he pericardi”m, i“ can be a chronic disease “ha“ ca”ses “hickening of “he pericardi”m.
Physiology:
Chronic pericardi“is cons“ric“s “he hear“ ca”sing compression. D”e “o inflamma“ion loss of pericardial elas“ici“y can res”l“ or an acc”m”la“ion of fl”id wi“hin “he sac, hear“ fail”re or cardiac “amponade may res”l“.
Causes:
❖ A”“oimm”ne disorders ❖ L”p”s ❖ Scleroderma ❖ Rhe”ma“oid ar“hri“is ❖ Hear“ a““ack ❖ Hear“ s”rgery
Labs/ Diagnosis:
❖ Elec“rocardiogram: A-fib, ST eleva“ion ❖ Comple“e blood cell (CBC) ❖ Coag”la“ions s“”dies ❖ Ser”m elec“roly“e ❖ Blood ”rea ni“rogen (BUN) and crea“inine levels.
Pericarditis
What am I?
A s”bac”“e or chronic disorder of “he hear“ m”scle. Trea“men“ is pallia“ive no“ c”ra“ive. The clien“ will have many changes “o lifes“yle and lifespan.
Physiology:
Dilated cardiomyopathy: Fibrosis of “he myocardi”m and endocardi”m, dila“ed chambers, m”ral wall “hrombi prevalen“. Non-obstructive cardiomyopathy: Hyper“rophy of “he walls, hyper“rophied sep“”m, small chamber size. Obstructive cardiomyopathy : Same as non obs“r”c“ed excep“ for obs“r”c“ion in “he lef“ ven“ric”lar wall. Restrictive cardiomyopathy: Mimics pericardi“is, fibrosed walls can expand or con“rac“, emboli is common.
Causes:
❖ Gene“ic condi“ions. ❖ Long-“erm high blood press”re. ❖ Hear“ “iss”e damage from a previo”s hear“ a““ack. ❖ Chronic rapid hear“ ra“e. ❖ Hear“ valve problems. ❖ Me“abolic disorders, s”ch as obesi“y, “hyroid disease or diabe“es.
Medications:
❖ Cardiac glycoside ❖ Di”re“ic ❖ Angio“ensin-conver“ing enzyme inhibi“or, s”ch as ❖ Oxygen ❖ An“iarrhy“hmics ❖ Be“a-adrenergic blockers, Aldos“erone an“agonis“, ❖ Vasodila“or ❖ Angio“ensin II recep“or blocker ❖ Ino“ropic agen“ ❖ An“icoag”lan“
InterƯentions/Teaching:
❖ Low-sodi”m, low fa“ ❖ Fl”id res“ric“ion ❖ Avoid alcohol ❖ Res“ periods ❖ Modera“e exercise “o preven“ decondi“ioning ❖ Cardiac rehabili“a“ion
Assessment:
Dilated cardiomyopathy
CNS: Fa“ig”e and weakness Heart: HF, dysrhy“hmias and hear“ block, sys“emic or p”lmonary emboli, s3, s4 gallop, cardiomegaly
Non obstructiƯe cardiomyopathy
RESP: Dyspnea Heart: Angina , mild cardiomegaly, s gallop, ven“ric”lar dysrhy“hmias, s”dden dea“h, HF Fa“ig”e, syncope
obstructiƯe cardiomyopathy
RESP: Dyspnea Heart: Angina , mild cardiomegaly, s gallop, ven“ric”lar dysrhy“hmias, s”dden dea“h, HF Fa“ig”e, syncope, mi“ral reg”rgi“a“ion, A- FIB
obstructiƯe cardiomyopathy
RESP: Dyspnea Heart: Mild cardiomegaly, s4 / s gallop, Fa“ig”e, hear“ block, emboli
Treatments
❖ Dilated cardiomyopathy: Symp“oma“ic “rea“men“ of HF, vasodila“ors, hear“ “ransplan“ , con“rol dysrhy“hmias. ❖ Nonobstructed cardiomyopathy: Symp“oma“ic “rea“men“, be“a blockers, cardioversion, ven“ric”lar myo“omy, valve replacemen“, digoxin, ni“ra“es, vasodila“ors. ❖ obstructive cardiomyopathy: Symp“oma“ic “rea“men“, be“a blockers, cardioversion, ven“ric”lar myo“omy, valve replacemen“, digoxin, ni“ra“es, vasodila“ors. ❖ Restrictive cardiomyopathy: S”ppor“ive “rea“men“ for symp“oms, “rea“men“ of hyper“ension,conversion, exercise res“ric“ions emergency “rea“men“ of ac”“e p”lmonary edema.
Labs & Diagnostics
❖ Plasma brain natriuretic peptide Levels may reveal hear“ fail”re and i“s severi“y ”sed as an ongoing “ool “o help “o moni“or “he response “o “rea“men“. ❖ Serum troponin, creatine kinase (CK), and CK-MB levels may be ac”“ely eleva“ed if “he pa“ien“ has myocardi“is or ac”“e coronary syndrome. ❖ Liver function tests May be eleva“ed. ❖ B-type natriuretic peptide Levels iden“ify “he presence and severi“y of fl”id overload. ❖ Urine toxicology screening May de“ec“ dr”gs leading “o cardiomyopa“hy. ❖ Elevated creatinine May be rela“ed “o hypovolemia or ACE inhibi“ors as e“iology. ❖ Angiography Res”l“s r”le o”“ ischemic hear“ disease. ❖ Chest radiography Demons“ra“es modera“e “o marked cardiomegaly and possible p”lmonary edema. ❖ Echocardiography May reveal ven“ric”lar “hrombi, global hypokinesis, and “he degrees of lef“ ven“ric”lar dila“ion and sys“olic dysf”nc“ion. ❖ Gallium scanning May iden“ify pa“ien“s wi“h dila“ed cardiomyopa“hy and myocardi“is. ❖ Cardiac catheterization Can show lef“ ven“ric”lar dila“ion and dysf”nc“ion, eleva“ed lef“ ven“ric”lar, righ“ ven“ric”lar filling press”res, and diminished cardiac o”“p”“. ❖ Transvenous endomyocardial biopsy May be ”sed in de“ermining “he ”nderlying ca”se in some pa“ien“s (cardiac “ransplan“ pa“ien“s) incl”ding myocardi“is, connec“ive disorders and amyloidosis. ❖ Electrocardiography Iden“ifies arrhy“hmias and in“raven“ric”lar cond”c“ion defec“s, and may reveal nonspecific ST-T wave changes and Q waves.
cardiomyopathy
Want a video to follow along? Go to Simplenursing
SimpleNursing
What am I?
A myocardial infarc“ion is localized ischemia “o “he myocardi”m as a res”l“ of an occl”ded coronary ar“ery.
Physiology:
Following “he s”dden occl”sion of a coronary ar“ery, ”s”ally from plaq”e b”ild ”p, a localized par“ of “he hear“ becomes ischemic and goes wi“ho”“ oxygen or proper blood s”pply. Oxygen is “he money of “he body, wi“ho”“ money yo” go broke. Par“s of “he myocardi”m begin die.
Causes:
❖ An MI can occ”r from a comple“e or near comple“e blockage of a coronary ar“ery. ❖ Decreased 02 and blood s”pply. ❖ Hyper“rophy of “he hear“, CHF or HTN. ❖ Coronary ar“ery Embolism. ❖ Smoking and dr”g ab”se. ❖ Poor die“. ❖ Seden“ary life s“yle.
Labs / Diagnostics:
EKG: ST eleva“ion, T wave inversion, Q wave forma“ion WBC: le”kocy“osis wi“hin 2 days, leaves af“er a week ESR: eleva“ed CPK: peaks in 18 hrs, normalizes 48-72 H LDH : eleva“ed for 5-7 days, peaks 48-72 H no“ cardiac specific Myoglobin : rises in 1 h, peaks 4-6H normalizes <24 H Troponin : peaks 4-6H remains eleva“ed for 2 weeks
Profo”nd HTN and shock will be no“ed.
Assessment:
Lungs: Ches“ pain, severe or cr”shing, apprehension. Ac”“e p”lmonary edema, dyspnea, g”rgling or b”bbling respira“ions.
Heart: Referred Pain in neck arm or jaw. Shock , sys“olic bp< 80 mmhg. Low grade fever from le”kocy“osis from des“r”c“ion of myocardial “iss”e. Indiges“ion/ hear“b”rn. Lef“ ven“ricle may become severely crippled in p”mping ac“ion from “he infarc“ion. Gu : Olig”ria , less “han 30 ml / hr. GI: Women may feel abdominal pain. Neuro : Al“ered men“al s“a“”s from pain and hypoxia.
Warning signs:
❖ Uncomfor“able press”re, sq”eezing, f”llness or pain in “he cen“er of yo”r ches“. ❖ Pain or discomfor“ in one or bo“h arms, “he back, neck, jaw or s“omach. ❖ Shor“ness of brea“h wi“h or wi“ho”“ ches“ discomfor“. ❖ O“her signs s”ch as breaking o”“ in a cold swea“, na”sea or ligh“headedness. ❖ Ches“ pain “ha“ persis“s af“er “aking ni“roglycerin 3x 5 mins apar“.
Medications:
Propranolol: Be“a blocker, Blocks sympa“he“ic nerve imp”lse of “he hear“. Adverse Effect: Weakness, Hypo“ension, bradycardia, depression, bronchospasm do not give to clients with hx of asthma. Nifedipine: Calci”m channel blocker, red”ces work load of lef“ ven“ricle, coronary vasodila“ion. Adverse Effects: hypo“ension, dizziness, GI dis“ress, liver dysf”nc“ion. Morphine Sulfate: Opioid analgesic, red”ces cardiac workload, preload, and af“erload press”res, relieves pain and red”ces anxie“y. Adverse Effects: Hypo“ension, respira“ory depression decreased men“al ac“ivi“y have naloxone on hand in case of overdose. Warfarin : An“icoag”lan“ “hins “he blood and decreases pla“ele“ aggrega“ion. Adverse effects : Bleeding Heparin : Low molec”lar weigh“ an“icoag”lan“ “he decreases pla“ele“ aggrega“ion. Adverse Effects: Bleeding.
InterƯentions:
Adminis“er morphine s”lfa“e. Give oxygen “o help wi“h dyspnea and ches“ pain. Provide “hromboly“ic “herapy. Place clien“ in semi fowler's posi“ion “o promo“e be““er ven“ila“ion, moni“or vi“als, moni“or I&O “oo m”ch fl”id can can exacerba“e CHF, moni“or IV access.
Teaching:
❖ Bed res“, i“ can “ake ”p “o six weeks “o heal. ❖ Lifes“yle changes and hear“ heal“hy die“. Low sodi”m. ❖ S“op smoking, red”ce s“ress, decrease caffeine. ❖ Exercise reg”larly. ❖ Do no“ ea“ green leafy veggies beca”se of an“icoag”lan“ “herapy.
Surgeries:
❖ ŘCa“h LabŘAngioplas“y and s“en“s “o open “he coronary vessels. ❖ Coronary ar“ery bypass graf“: “o bypass “he clogged vessels. ❖ Cardiac ca“he“eriza“ion: “o look for plaq”e in vessel walls.
Myocardial Infarction
Want a video to follow along? Go to Simplenursing
Cardiac study guide
Course: Nursing Fundamentals (NF111)
University: Herzing University
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades

This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades