- Information
- AI Chat
Mental Health Midterm Study Guide
Nursing And The Promotion Of Mental Health (NRSG 3400)
Northeastern University
Recommended for you
Related Studylists
NURS116Preview text
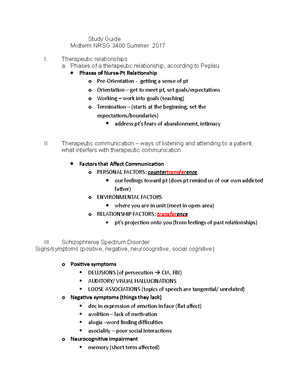
Mental Health Midterm Study Guide Maslow’s Hierarchy of needs o Physiological needs always comes first
o Nursing process o Assessment Look at affect and symptoms o Diagnosis o Identify outcomes/goals Decide goals Patient must be included in the goals o Plan o Implementation What they do first Need to assess first before intervention o Evaluate Assess- this is a cycle not a flow chart Phases of a nurse-patient relationship posited regard built off of Sullivan o Hildegard Pepleau Pre-orientations Planning schedule Orientation Intake Getting to know patient Contracts and limitations Intake- can last several sessions Rapport building Boundary setting Counteract (formal/informal-terms of termination) confidentiality o Limits Mandated reporting If a child, developmental disabilities Children is dcf 51A
BBS disabilites o Requirements o Mandatory reporting Working phase Role of the nurse- still building Implanting care plans Working to achieving Termination Because patient getting better Start during orientation phase at the beginning Basics of mental health o Transference Relationship between nurse and the patient that relates like o Countertransference How nurse feels about the patient Nurse does not act from own experience Need to keep in check so it doesn’t interfere o Confidentiality (releases) Mandated Reporting Kids, adults over 60, disabilities GIVING INFORMATION INFORMED CONSENT Unless section 12, court ordered Substance abuse is section 35 If the patient tells about hurting self o Interpreters/Culture o Therapeutic Communication Reality testing (do you see things I can’t see?) Are you seeing things or seeing things they may not resepond to do you or are you o Validation Sounds like you are really missing your daughter Do not join delusion o Safety Safety Safety Danger to self and others Section 12 Section 35 Theories o Pepleau- 4 stages therapeutic work to decrease anxiety 4 stages Pre-orientation phase: each member are getting to know each other o Reading chart Orientation phase: developing goals
o Skinner: behaviorism Operant conditioning: poisitve reinforecemnt for behaviors Positive and negative reinforcement o Negative not used as much NOTE: skinner=skinny behavior. You can get a cookie if you lose some weight as positive reinforcement o Freud: psychoanalytic ID, Ego, superego ID: instincts and drive (bottom of the iceberg) Ego: in the middle Superego: societal norms Transference and countertransference Transference: patient projects feeling onto nurse as if they are interacting with someone from the past Countertransference: feeling or actions of the nurse put onto the patient o Nurse with alcoholic father may not like the alcoholic patient o Beck: cognitive theory
Looks ar how person feels and behaves is based on perspective of the world Conditions: way of thinking- verbal or pictoral events in one’s conscious experience Schemata: attitudes and assumptions Ex: if pt makes dinner date, then friend forgets, the pt assumes the friend does not like them NOTE: Beck=back- watch your back and look at how someone feels. Then you have the schemata if your friend ditches you Types of care o Outpatient Majority of cares Higher level of care o Intensive outpatient (parioal- IOP) Structured during the day group based Returns home at night o HOME SERVICES/csa For kids and complex patients o Cbat- community based acute treatment Kids is non lock unit All voluntary o Inpatient setting Voluntary Involuntary Section 12 or 35 Cannot leave on their own Hard to build trust Bipolar Disorder o Bipolar 1 Fluctuation of mania and depressive episodes Two week or more episodes of mania and depression Symptoms o Bipolar II Major depression, hypomania, timing less defined Does not reach mania level Time less defined Patients get treatment during depressive phase
o Cyclothymic- Sub diagnostic clinical symptoms Rapid cycling- prevalent with kids Clincial symptoms are sub criteria o Causes Genetic (huge influence) Environment Hormonal/Neurobiological Stress/Diathesis stress model
o Acne Nursing considerations: narrow therapeutic window leads to toxicity o Symptoms of toxicity: tremors, N/V/D, ataxia/confusion, poor coordination, polydipsia/urea. Slurred speech, muscle weakness o Take with meals to limit GI upset Labs for lithum: 0.8mEq/L-1/L o Check kidney function, thyroid and EKG Lithium takes the place of sodium in kidney Need to hydrate properly o Check symptoms o Kidney lithium takes place of sodium o If complaint of GI take with food o Lithium is soluble and needs to be hydrated If dehydrates toxicity can develop Anticonvulsants Triletal/tegretal/Depakote/Lamictal o Steven johnson syndrome with Lamictal Rash and allergic reaction Autoimmune rash Life threatening Atypical antipsychotics Seroquel/Risperdal/Geodon/Abilify/Latuda o May lead to metabolic syndrome Leads to weight gain/disturbed body image Increased blood sugar a1c Hyperlipidemia o Don’t have twitches o Careful with type Ii diabetes CAUTION WITH SSRIs- rapid cycling, shift to mania If suspect bipolar use SSRI first Black box warning: suidicidal in younger people o Controversial because suicide rate is low o Bipolar treatment Encourage patient to adehere to medication If people feel better they may not be as adherent Encourage individual and family therapy Group therapy is helpful, but challenging during mania Maintain safety of all patients Respect and rely on the therapeutic relationship Remain non-judgemental /Use distraction, avoid power struggles Hold staff meeting to support each other and maintain consistent care with patient Depressive disorders
o Types Major depressive disorder: prolonged sad or depressed mood that causes a decrease in function Longer than 6 weeks Older adults have difficulty o Especially in differ t problems o Think of as weak if they seek care Single episode Recurrent episode Lifelong chronic condition Dysthymic do not meet criteria Subtypes can have psychosis Have unclear symptoms o Characteristic Vegetative symptoms (over-sleeping/eating, depressed mood) Change in weight PPD post partum With psychosis is not as common SAD- atypical symtpms, light therapy seasonal Lack of light o Use light therapy Use SSRI/ SNRI o Wellbutrin o Symbalta Comorbidities can be present Anxiety, ADHD Disturbances in sleep, appetite, concentration issues, some issues with executive functioning o Special populations Elderly Highest risk for completing suicide- men over 60 o Especially access the firearms o Women have more attempts When differentiating diagnosis, treat depression before diagnosing dementia o Cognitive changes can occur with dementia Children/Adolescents Irritability Anhedoni a-refusing to engage in previously enjoyed activities o Very concerning o All of a sudden does not want to go to school and somatic complaints Somatic Complaints School Phobia Black Box warnings on SSRI’s o Assessment
Zolof with OCD Caution if patition has history of bipolar, monitory for increased suicidal thoughts o Do not want to send them into mania Black box warning o Make sure to informed consent SNRI Caution in those with seaizures Meds can lower seizure thresholds TCA amatryptsline Check for arrythmias o Baseline ekg Sedating MAOI Older but rarely used Has dietary restrictions Ingesting tyramine can cause hypertensive crisis o Dark chocolate, smoked meat o Ask what they eat in the past few days because the medications have long half life Defense mechanism people become distressed when they o Common Denial Believing it is not he opening Smokers may refuse to admit to themselves that smoking is bad for them Alcoholic who is going to AA but still drinking Projection Project onto another situation. You might hate someone, but your superego tells you that such hatred is unacceptable. You can solve the problem by believing that they hate you Displacement (mad at spouse but yells at kids) Someone who is frustrated with his boss at work may go home and kick the dog Repression - stuffing, mad at boss- forgert a meeting Stuff deep inside Regression - prior stage immature behavior less demands- self soothing Go into young state Act young where there were no worries Sublimation - mad at neighbor, want to punch them start painting garage instead Sport is an example of putting out emotions/aggression into something constructive reaction formation - keeping your enemies close
Fake it til you make it Aware of what you are feeling In repression you do not think anything is wrong Two coworkers fight all the time because they actually are attracted to each other o Treatment CBT strong edict base Thoughts effect behavior o Help to restore future o 8-12 weeks before SSRI Individual Group o Helping patient restore function and be future oriented Transcranial magnetic stimulation After vegetative depression Day procedure Ketamine- trials Nasal spray For depression ECT Seem invasive but can be life changing For depression treatment resistant Schizophrenia o Characteristics Brain abnormalities Decreased grey matter Excessive and decreases in neurotransmitters are thought to be responsible o Dopamine thought to be cause Genetic predisposition- family history, separated twin studies First break is usually in the 20’s around a milestone or stressful time Can occur in childhood, but rare Rare in later adulthood to develop o Women have older onset than men o Types Schizo-affective disorder Disorder has symptoms and characteristics of both schizoaffective disorder and manic/mood symptoms of bipolar disorder but the patient does not meet full criteria of either. Does not meet criteria for schizophrenia or bipolar Usually treated with antipsychotics Comorbidites common with schizophrenia Must treat symptom set o Symptoms Posive symptoms Delusions (FBI spying, authority)
o IM meds Medication often more helpful with managing positive symptoms vs. negative symptoms Hopes to prevent relapse Community supports (SSI, SSDI, VNA services, guardians) Monitor for self medication with substances- common co-morbidity. ETOH very common o Medications Atypicals Zyprexa, risperfal, Geodon, Seroquel, Abilify Clozaril o Last resort because of agranulocytosis Careful with metabolic syndrome o Even more with nutrition Fist generation Haldol, prolizen, trilafon, Thorazine o Haldol given often Side effects o Muscle stiffness, tardive dyskinesia, sedation Thorazine shuffle o Akathisia o Anticholinergics cause Pseudo parkinsonism- tremor, muscle stiffening, shuffling gait o Acute dystonic reactions: acture sustained muscle contractioning often starting with the neck of jaw With many first generation medication
Mental Health Midterm Study Guide
Course: Nursing And The Promotion Of Mental Health (NRSG 3400)
University: Northeastern University

- Discover more from: