- Information
- AI Chat
Health Assessment Final Review
Foundations Of Health Assessment (NUR 3029)
Nova Southeastern University
Recommended for you
Preview text
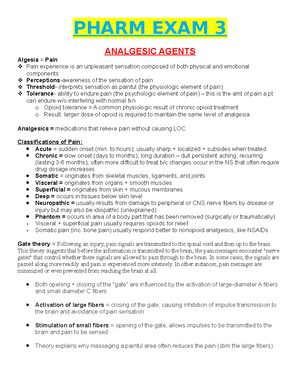
Pain:
Complex and subjective that originates from the CNS or PNS or both.
Nociceptors: detect pain sensations from periphery and transmit to the CNS
o A delta: myelinated, transmit pain signal faster
o C fibers: unmyelinated, transmit pain signal slower
Neuropathic: hardest to assess and treat, comes from damage or injury to nerve fibers and is perceived long after the site of injury has heals around 2-3 years later.
Acute/ Chronic:
o Acute: short term example: surgery, trauma, or kidney stones
o Chronic: persistent long term pain 6 months or longer it can last beyond 20 years, can be malignant or nonmalignant example: tumors.
Gender/Culture:
o Gender: influenced by societal expectations, hormones, and genetic makeup. Traditionally men have been raised to be more stoic than women. Hormonal are found more painful on women.
o Culture: various studies show that black and Hispanics are often prescribed and administered less analgesic therapy than whites.
Subjective/Objective:
o Subjective: ask patient if they have any pain, if the answer is yes; ask patient to rate pain on a scale,
-Intensity Scale (numerical): children after 5 years and adult’s rates from no pain to severe pain -Face Pain Scale: for infants and children, from smiling face to frowny face o Objective: patient shows they are in pain but may not say it such as grimacing, crouching, fetal position, guarding of the area, moaning, agitation, moodiness, diaphoresis (sweating) change in vital (increase HR, BP, RR), crying etc.
Pain assessment
P = Provocative or palliative - What brings on the pain? What were you doing when you noticed it?
Q = Quality or quantity - How does it look, feel, sound?
R = Region or radiation - Where is it? Does it spread anywhere?
S = Severity scale: 1 to 10- How bad is the pain? Rate the pain for me.
T = Timing or onset - Onset: When did it first occur? Duration: How long did it last? Frequency: How often does it occur?
U = Understand patient’s perception of problem- What do you think it means?
Assessment Technique
INSPECTION: it is close careful scrutiny, first of the individual as a whole and then of each body system. o When to use it: -Assess for symmetry, color
o How its done: By observing and not touching patient PALPATION o When to use it: To assess for: texture, temperature/ moisture, organ location/size, swelling, vibration/pulsation, rigidity/spasticity, crepitation, lumps/mass, tenderness/pain. o How to use it: Light: for surface Deep: for size, density, tenderness Bimanual: to cup a body part or organ Fingertips: for fine tactile discrimination; skin texture, swelling, pulse, and lumps Grasping of finger and thumb: for position, shape, and consistency of organ or mass Base of fingers: vibrations The dorsa (backs) of hands & fingers- best for determining temperature because the skin here is thinner than on the palms PERCUSSION o When to use it: to asses for vibrations, locations and size o How to use it: Stationary hand: place your dominant hand flat and hyperextended on patient Striking hand: use middle finger of dominant hand as the one to strike. With your striking hand use both index and middle finger to strike Directly: striking hand to skin Indirectly: striking hand to dominant hand o Types Resonant: pitch- low, Normal lung tissue Hyperresonant: pitch-lower, abnormal amount of air in adult Tympany: pitch-drum, air filled stomach/ intestine Dull: pitch-high, over dense organ ex: liver/ spleen Flat: pitch-high, ex: muscle, bone, tumor AUSCULTATION o Why do you use it: to assess and note any abnormal sounds the person may have o How: Using a Stethoscope with a bell and diaphragm and occasionally a Doppler.
Stethoscope: listening device for heart, vessels, lungs, and abdomen
Diaphragm: best for high pitched sounds such as: breaths, bowel and normal heart sounds Bell: hollow cup like shape and is best for soft low pitched sounds such as: extra heart sounds or murmurs and blood vessels.
Otoscope: funnels light into the ear canal and onto the tympanic membrane.
Ophtalmoscope: illuminates the internal eye structures.
What do you hear in each body system?
What do you feel in each body system?
Vital signs
Temperature
Head and neck
Size and shape
Normal: skull feels normocephalic, which means its round, symmetrical and appropriate to body size.
Abnormal:
Deformities: Microcephaly:
Abnormally small head.
Macrocephaly: abnormally large head.
Note lumps, depression or abnormal protrusions
Temporal Area
Normal: Palpate artery just above the zygomatic bone between the eye and top of the ear Palpate temporomandibular
joint which is located below the temporal artery and the temporal artery and anterior to tragus, palpate the joint as
the person opens mouth and note normally smooth movement with no limitations or tenderness.
Abnormal:
The artery looks tortuous, feels hardened and tender with temporal arteritis.
Crepitation, limited ROM or tenderness.
Older Adult:
Normal: Temporal arteries are twisted and prominent, tremors, and tongue protrusion. Sunken-in mouth due to loss
of teeth. Prolapse of submandibular glands are normal and sometimes mistaken as tumors.
Facial structure
Normal: symmetrical, expression appropriate with behavior.
Abnormal:
Note any abnormal structures or swelling and involuntary movements of the facial muscles.
Grinding of jaws, tics or excessive blinking.
Tense, rigid muscles indicate anxiety or pain.
Mark as asymmetry with central brain lesion or with peripheral cranial nerve VII.
Edema in the face occurs around the eyes first
(periorbital)
Lymph Nodes
Assessment: Palpation of the lymph nodes is used with a
gentle and circular motion of your finger pads with gentle
pressure comparing symmetry.
Begin with the preauricular lymph nodes and palpate the 10
groups in order. If any nodes are palpable note their location,
size, shape, delimitation, mobility, consistency and tenderness
Normal: nodes feel movable, discrete, soft and non-
tender. Normally the salivary glands are not palpable
Abnormal: Lymphadenopathy is the enlargement of
the lymph nodes from infection allergy or neoplasm.
Parotid enlargement has been found with AIDS.
Swollen parotid is with mumps. Clumped lymph node is indicative of tuberculosis. Unilateral, non-tender
and fixed is indicative of cancer. Occipital node enlargement is usually HIV. Rubbery and discreet lymph
nodes are indicative of Hodgkin’s lymphoma.
Thyroid
Assessment: Palpation to assess the thyroid is used to check for enlargement, consistency, symmetry and the
presence of nodules. It is used in two different ways:
Posterior approach : stand behind the person and have them bend their head to the right. Use your left fingers
to push trachea to the right and your right fingers to retract the sterno-mastoid muscle. Ask the person to
swallow and assess.
Anterior approach : stand facing the person and ask if they can tip their head to the right. Use of RT thumb to
displace the trachea to their right. Place your LT thumb and fingers around the sterno-mastoid muscle and as
the person swallows, assess.
Auscultation is used to listen for a bruit. A soft, pulsatile, whooshing, blowing sound.
Abnormal: Enlarged lobes that are easily palpated before swallowing or tender to palpation. Presence of nodules or
lumps, bruit while auscultating the thyroid.
Tonsils
Assessment Normal Abnormal
The tonsils are inspected and graded in size as follows: 1+ Visible. 2+ Halfway between tonsillar pillars and uvula. 3+ Touching the uvula. 4+ Touching each other.
You may normally see a 1+ or 2+ tonsils in healthy people, especially in children because lymphoid tissue is enlarged until puberty. The normal color is the same pink as the oral mucosa. There should be no exudates on the tonsils.
Tonsils are enlarged with to a 2+, 3+, 4+ with an acute infection. With an acute infection, tonsils are bright red and swollen and may have exudates or large white spots.
Oral Mucosa Assessment Normal Abnormal Lips Inspect the lips for color, moisture, cracking or lesions. Retract the lips and note their inner surface as well.
all racial groups have lips that are deeper or pinker than facial skin, however some African Americans have normally bluish lips and a dark line on the gingival margin
Cheilitis or cracking at the corners. Herpes or other lesions. Circumoral pallor: shock or anemia Cyanosis: hypoxemia and chilling Cherry red lips: carbon monoxide or aspirin poisoning and ketoacidosis. Teeth and Gums
Inspect for any diseased, absent, loose or abnormally positioned teeth. Inspect the gums for swelling, retraction of gingival margins, spongy, bleeding, or discolored gums.
Teeth normally look white, straight, evenly spaced and clean and free of debris or decay. Normally the gums look pink or coral with stippled surface. Gum margins are tight and well defined.
Gums bleed with slight pressure indicate gingivitis. Dark line on gingival margins occurs with lead and bismuth poisoning. Grinding down of tooth surface, plaque, caries, decay. Tongue Assess the tongue for color, surface characteristics and moisture. Ask the patient to touch the roof of the mouth with the tongue and assess the ventral surface. With gloves hold the tongue and swing it to both sides and inspect for any white patches or lesions. Inspect under the tongue behind the teeth.
The color is pink and even. The dorsal surface is normally roughened from the papillae. The ventral surface should look smooth and glistening and shows veins and saliva. No lesions should be present at the sides or under the tongue.
Beefy red, swollen tongue. Enlarged tongue occurs with mental retardation, hypothyroidism, acromegaly. A small tongue is with malnutrition. Dry mouth occurs with dehydration and fever. Any lesions or ulcer lasting more than 2 weeks should be investigated. Buccal Mucos a
With a wooden tongue blade, check and inspect the buccal mucosa for color, nodules or lesions.
It should look pink, smooth, moist. Fordyce granules are papules on the mucosa and now painless and not significant.
Dappled brown patches are present with Addison disease. Orifice of stensens duct looks red with mumps. Koplik spots are early signs of
Direct light reflex occurs (constriction of the pupil at same time/ same side) Consensual light reflex (simultaneous constriction of the other pupil)
Accommodation: adaptation of the eye for near vision, accomplished by increasing the curvature of the lens through mvmt of the ciliary muscles. Although the lens cannot be observed directly, the components of accommodation that can be observed are convergence (motion toward) of the axes of the eyeballs and papillary constriction. Adaptation of the eye for near vision Distant- dilatation Near- constriction Convergence of axes Expected finding for accommodation: convergence and pupil constriction (with use of penlight)
Iris & Pupil pg 295 The iris normally appears flat with a round regular shape and even coloration. Note the size, shape, equality of the pupils. Normally the pupils appear round, regular and of equal size in both eyes. In the adult, resting size is from 3-5 mm. a small # of ppl (5%) normally has pupils of 2 diff sizes, which is termed anisocoria.
To test the papillary light reflex, darken the room and ask the person to gaze into the distance. (This dilates the pupils) advance a light in from the side and the note the response. Normally you will see:
- constriction of the same sided pupil (direct light reflex)
- simultaneous constriction of the other pupil (consensual light reflex) In the acute care setting, gauge the pupil size in mm, both before and after the light reflects. Recording the pupil size in mm is more accurate when nurses and physicians care for the same person or when small changes may be significant signs of increasing intracranial pressure. Normally the resting size is 3, 4, 5 mm and decreases equally in response to light.
Test for accommodation by asking the person to focus on a distant object. This process dilates the pupils. Then have the person shift gaze to a near object, such as your finger held abt 7-8 cm (3”) from the person’s nose.
- A normal response includes: pupillary constriction and convergence of the axes of the eyes.
Record the normal response to all these maneuvers as PERRLA or Pupils: inspection Equal: inspection Round: inspection React to: (penlight) pupillary light reflex Light and Accommodation: test Know which test to use for each letter****
Irregular shape Although they may be normal, all unequal size pupils call for a consideration of central nervous system injury. Dilated pupils Dilated and fixed pupils Constricted pupils Unequal or no response to light
Absence of constriction or convergence. Asymmetric response.
Extraocular Muscle function
Diagnostics Positions Test pg 291 (Inspect EOM fxn)
Leading the eyes through the 6 cardinal positions of gaze (CN III, IV, VI) will elicit much muscle weakness during mvmt. Ask the person to hold the head steady and to follow the mvmt of your finger, pen or penlight only with the eyes. Hold the target back abt 12” so the person can focus on it comfortably, and move it to each of the 6 cardinal positions, hold it momentarily, then back to center. Progress clockwise. A normal response is parallel to tracking of the object w/ both eyes.
Eye mvmt is not parallel.
Failure to follow in a certain direction indicates weakness of an extraocular muscle (EOM) or dysfxn of CN innervating it.
Cover/Uncover Test
Cover Test (Inspect EOM fxn) Detects small degrees of deviated alignment by interrupting the fusion
If eye jumps to fixate on the designated point it was out of alignment before.
reflex that normally keeps the two eyes parallel. Ask the person to stare straight ahead at your nose even though the gaze may be interrupted. With an opaque card cover one eye. Meanwhile the macular images have been suppressed on the covered eye. If muscle weakness exists, the covered eye will drift into a relaxed position. Now uncover the eye and observe it for mvmt. It should stare straight ahead. If it jumps to reestablish fixation, eye muscles weakness exists. Repeat with other eye.
A phoria is a mild weakness noted only when fusion is blocked A tropia is more severe, a constant malignant of the eyes.
- Glaucoma: o Build up of intraocular pressure affecting the optic nerve (CNII) o Open-angle glaucoma (chronic open angle is the most common): fluid builds up because there is a clog in the inner canals but it is very slow progressing and painless. In this case, peripheral vision loss is seen and progressively becomes worse until the person begins to experience tunnel vision. o Closed-angle glaucoma: blockage that occurs suddenly and is an emergency. It is painful and sudden. Halos/rings are noted in the person’s vision. If left untreated a person can lose vision within 2-3hrs
Handheld eye chart testing vs Snellen Chart
Snellen Eye Chart (test central visual acuity)
(measures distance) pg 287 (which nerve would you use to test To measure acuity = CN II)
The snellen alphabet chart is the most commonly used and accurate measure of visual acuity. It has lines of letters arranged in decreasing size. You place the snellen alphabet chart in a well-lit spot at eye level. Position the person on a mark exactly 20 feet from the chart (distance). Hand over an opaque card with which to shield one eye at a time during the test; inadvertent peeking may result when shielding the eye the persons own fingers. If the person wears glasses or contact lenses, leave them on. Remove only reading glasses because they will blur distance and vision. Ask the person to read through the chart to the smallest line of letters possible, encourage trying the smallest line also.
Record the result using the numeric fraction at the end of the last successful line read. Indicate if the person missed any letters or if corrective lenses word for example, right 20/30 – 1 with glasses. That is the right eye scored 20/30 missing 1 letter.
Normal visual acuity is 20/20, contrary to some people impression; the numeric fraction is not a % of normal vision. The top (numerator) # indicates the distance the person is standing from the chart, and the bottom # (denominator) gives the distance at which a normal eye could have tread that particular line.
i.: 20/30 means you can read at 20 feet what the normal eye can see from 30 feet away
If the person is unable to see the largest letters, shorten the distance to the chart until it is seen and record the distance (e. 10/200) If visual acuity is even lower, assess whether the person can count your fingers when they are spread in front of the eyes or distinguish light perception from your penlight.
Note hesitancy, squinting, leaning forward, and misreading letters.
The larger the denominator (bottom) the poorer the vision. If vision is poorer than 20/30 refer to an ophthalmologist or optometrist. Impaired vision may be due to refractive error, opacity in the media (cornea, lens, vitreous), or disorder in the retina or optic pathway.
Near vision (test central visual acuity)
For 40+ or those who report increasing difficulty reading, test near vision with a handheld vision screener with various sizes of print. Hold the card in
Presbyopia: the decrease in power of accomodation with aging, is suggested when the person moves the card farther away
{When pt has hearing loss they will usually stare at your lips to read what you are saying because they cannot hear
you}
Health history questions:
Biographic data
Age 20-40y otosclerosis
Gender
Current health status:
Hearing loss-
Hearing loss- slowly or all at once? Decreased all the time or just with certain sounds?
Vertigo-originates with the person; TRUE vertigo– true rotational spinning occurs with an
affected/dysfunction labyrinth
Subjective- feels like the person is spinning – true vertigo
Objective- feels like the room is spinning
This distinguishes true vertigo from dizziness or light-headedness
Tinnitus- originates within the person; it accompanies some hearing or ear disorders. Ringing/buzzing of the
ears; seems louder with no competition from outside noise Many meds have ototoxic sequelae: aspirin,
aminoglycodisdes (streptomycin, gentamic, kanamycin, ... if pt is in hospital you need to be aware of
meds/antibiotics because they can cause this)
Otorrhea - Ear drainage- discharge: infected canal or perforated eardrum such as:
(love note: know that of the 3, they have diff color drainage)
External otitis: purulent, sanguineous or watery discharge
Acute otitis media with perforation: purulent discharge (typically with perforation ear pain occurs
first, stops with a popping sensation, then drainage occurs)
Cholesteatoma: dirty yellow/gray discharge foul odor
Otalgia Ear ache – may be directly due to ear disease or may be referred pain from a problem in teeth or
oropharynx. Virus/ bacteria from upper resp infection may migrate up the Eustachian tube to involve the
middle ear. Trauma may rupture the tympanic membrane.
Past health history:
History of frequent ear infections as a child:
1st episode before 3 mo- increases risk for recurrent OM
Recurrent OM- more than 3 episodes in 3-4 months
Exposure to second hand smoke as a child
*Love note: “OM, furnacle, and OE all cause pain”
The External Canal Note the color and odor if
any discharge is present.
For patients with hearing
aids, note any irritation on
the canal wall.
-Otitis Externa-redness
and swelling occurs, canal
may be completely closed
with swelling.
-Purulent otorrhea
suggests otitis externa or
otitis media if drum has
ruptured.
-Frank blood or clear,
watery drainage (CSF)
after trauma suggests
basal skull fracture and
warrants immediate
referral. CSF feels oily and
is positive for glucose on
TesTape
-Foreign body, poly,
furuncle, exostosis.
Hold your otoscope “upside down” along your
fingers and have the dorsa (back of your hand)
along the person’s cheek braced to steady the
otoscope.
Insert the speculum slowly and carefully along
the axis of the canal, watch the insertion; then
put your eye up to the otoscope. Avoid
touching the bony section of the canal wall.
Perform the otoscopic examination BEFORE
you test hearing
Ear canals with impacted cerumen give the
erroneous (invalid) impression of pathologic
hearing loss.
The external canal:
Note any redness swelling, lesions, foreign
bodies, or discharge. If any discharge is present,
note the color and odor. (also clean any
discharge from the speculum before examining
the other ear to avoid contamination with
infectious material) for a person with a hearing
aid, note any irritation on the canal wall from
poorly fitting ear molds.
Tympanic membrane:
Color and characteristics – normal eardrum is
shiny and translucent, w/ pearl gray color.
The cone shaped light reflex is prominent in the
anteroinferior quadrant (@ 5 o’clock position in
the r. drum and the 7 o’clock position in the l.
drum) This is the reflection of your otoscope
light.
Position – eardrum is flat slightly pulled in at
the center and flutters when the person performs
the valsalva maneuver or holds the nose and
swallows.
Avoid with aging person as may disrupt
equilibrium and with upper resp infection bc it
could propel infectious matter into middle ear.
Redness and swelling can occur with otitis externa (OE);
canal may be completely closed with swelling.
Purulent otorrhea suggests otitis externa (OE) or otitis
media (OM) if the drum has ruptured.
Frank blood or clear watery drainage (cerebrospinal fluid
{CSF}) after trauma suggest basal skull fracture and calls
for immediate referral
~>Basal skull fracture = emergency
CSF feels oily- + for glucose on TES TAPE
Foreign body, polyp, furuncle, exostosis.
“Does ear normally have drainage in it/coming out of it? Not normally but a trauma that creates drainage of the ear can indicative of a basal fracture and can be indicative of CSF leaking if the fracture is deep enough indicative of a medical emergency. CSF bathing the brain.”
Yellow-amber drum color occurs with otitis media with
effusion (serous)
Red color with acute OM – common abnormality
Absent or distorted landmarks
Air/fluid level or air bubbles behind drum indicate otitis
media with effusion.
Retracted drum from vacuum in middle ear w obstructed
Eustachian tube.
Bulging drum from increased pressure in the OM
Drum hypomobility is an early sign of OM
Perforation shows as a dark oval area or as larger opening
on the drum.
TEST HEARING ACUITY
Screening for a hearing deficit begins during the
history
Whispered voice test – Test one ear at a time
while masking hearing in the other ear to
prevent sound transmission around the head.
This is done by placing 1 finger on the tragus
and rapidly pushing it in and out of the auditory
meatus. Shield your lips so the person cannot
compensate for a hearing loss by lop reading or
pushing the “good ear”. With your head 1 to 2
The person is unable to hear the whispered items. A
whisper is a high-frequency sound and is used to detect
high tone loss.
Abnormal : unable to repeat words/unable to hear
whispered items.
A whisper is a high frequency sound
used to detect high tone loss
Atresia: absence or closure of the ear canal
ft from the person’s ear exhale and whisper
slowly a set of 3 random #’s and letters.
Normally the person repeats each #/letter
correctly after you say it. If the response is
not correct repeat the whisper test using a
combo of 3 different of 3 #/letters. A passing
score is correct repeating of at least 3 out of a
possible 6 #/letters. Assess the other ear using
yet another set of whispered items.
Normal : pt repeats what you said
Chronic OM relieved by tympanostomy tubes
Musculoskeletal Assessment
Phalens test To check for carpel tunnel o Ask the person to hold both hands back to back while flexing wrist at 90 degrees. o Normal: acute flextion of wrist for 60 sec. no symptoms o Abnormal: produces numbness and burning.
Tinel sign To check for carpel tunnel o Percuss directly on the location of median nerve on wrist o Normal: no symptoms o Abnormal: burning and tingling
Ballottement of the patella (fluid test) Use left hand to compress the suprapatellar pouch to move any fluid into the joint. With your right hand, push the patella sharply against the femur o Normal: no fluid= patella snug against femur o Abnormal: if fluid you tap on patella and it moves through fluid and you can hear it tap as it bumps into femur
McMurray test To check torn meniscus o Hold the heel and flex the knee and hip. Place your hand on the knee with fingers on the medial side. Rotate the leg in and out to loosen the joint. Slowly extend the knee Leg extend smoothly with no pain Abnormal: if you hear or feel a click the test is positive for tear.
Kyphosis: Hunchback/ hump back, accentuated thoracic curve Occurs in older adults Lordosis: Accentuated lumbar curve, creating strain in lower back muscles
First, assess patency by occluding one nostril at a time and asking the person to sniff. With person’s eyes closed, occlude one nostril and present an aromatic substance that is familiar and non-noxious smells (coffee, toothpaste, orange, vanilla, soap, or peppermint, alcohol wipes are easy to find but irritating). Normal: can identify odor on each side of the nose. Normally decreased bilaterally w/ aging.
Anosmia- decrease or loss of smell occurs bilaterally w/ tobacco smoking, allergic rhinitis, & cocaine use Neurogenic anosmia- unilateral loss of smell in the absence of nasal disease
CN II Optic Test: Visual acuity- Snellen Chart Visual fields- Confrontation Using ophthalmoscope, examine ocular fundus to determine color, size, & shape of optic disc
Visual field loss Papilledema (swelling of optic disc) with increased intracranial pressure; optic atrophy
CN III, IV, VI Oculomotor, Trochlear, Abducens Palpebral fissure usually equal in width or nearly so Pupils: o Size, regularity, equality o Direct/consensual light reaction o Accommodation EOM by cardinal positions of gaze Normal: (nystagmus is a back-and-forth oscillation of eyes). End-point nystagmus, a few beats of horizontal nystagmus at extreme lateral gaze Assess any other nystagmus: o Presence in one or both eyes o Pendular movement (oscillations move equally left to right) or jerk (a quick phase in one direction, then a slow phase in the other). o Amplitude (fine, medium, or coarse) o Frequency (constant or fades) o Plane of movement (horizontal, vertical, rotary or a combination)
Ptosis (drooping of upper eyelid)- occurs w/myasthenia gravis, dysfunction of CN III, or Horner syndrome Increasing intracranial pressure causes a sudden, unilateral, dilated, & nonreactive pupil Strabismus (deviated gaze) or limited movement; cross eyed or lazy eye Nystagmus- occurs w/ disease of vestibular system, cerebellum, or brainstem
CN V Trigeminal Motor (mastication) Palpate temporal and masseter muscles as the teeth are clenched. Should feel equally strong on both sides. Next, try to separate jaws by pushing down on the chin; normally you cannot. Sensory (light touch sensation) With person’s eyes closed, touch these areas on face w/ a cotton wisp: forehead, cheeks, & chin. Ask person to say “Now” when touch is felt. Tests all 3 divisions of nerve: ophthalmic, maxillary, mandibular Corneal reflex (tests CN V and CN VII) Omitted unless person had unilateral sensorineural hearing loss
Decreased strength on one or both sides Asymmetry in jaw movement Pain with clenching teeth
Decreased or unequal sensation. w/ stroke, sensation of face & body is lost on opposite side of lesion
Test is limited clinically because an absent blink
Bring cotton wisp in from side, touch cornea. Note bilateral blink reflex. Normal: may be decreased or absent w/ contact lens & aging people
occurs w/ acoustic neuroma and a large tumor
CN VII Facial Motor (mobility and facial symmetry) Note responds to : smile, frown, close eyes tightly (against your attempt to open them), lift eyebrows, show teeth, & puff cheeks. Then press the person’s puffed cheeks in and note that air should escape equally from both sides Sensory (taste) Do not test routinely; only when facial nerve injury is suspected Apply cotton applicator covered w/ sugar, salt, or lemon juice to the tongue. Ask person to identify.
Muscle weakness shown by flattening of nasolabial fold, drooping of one side of face, lower eyelid sagging, and escape of air only from one cheek that is pressed in Loss of movement and asymmetry of movement occur w/ both CNS lesions (ex: brain attack or stroke that affects the lower face on one side)& PNS lesions (ex: Bell’s palsy that affects upper & lower face on one side)
CN VIII Acoustic/ Vestibulocochlear Test hearing acuity by the ability to hear normal conversation Whispered voice test CN IX and X Glossopharyngeal and Vagus Motor (gag reflex, phonation, swallowing) Depress tongue w/ a tongue blade & note pharyngeal movement as the person says “ahh” or yawns; uvula and soft palate should rise in the midline, and tonsillar pillars should move medially Touch posterior pharyngeal wall w/ tongue blade and note gag reflex Sensory (taste) CN IX mediates taste on posterior 1/3 of tongue, but difficult to test
Absence or asymmetry of soft palate movement or tonsillar pillar movement. Following a stroke, dysfunction in swallowing may increase risk for aspiration. Hoarse or brassy voice occurs w/ vocal cord dysfunction; nasal twang occurs w/ weakness of soft palate
CN XI Spinal Accessory Examine sternocleidomastoid and trapezius muscles for equal size. Check equal strength by asking person to rotate head forcibly against resistance applied to the side of the chin. Then ask person to shrug shoulders against resistance. Movements should feel equally on both sides
Atrophy Muscle weakness or paralysis occurs w/ a stroke or following injury to the peripheral nerve (ex: surgical removal of lymph nodes)
CN XII Hypoglossal Inspect tongue, no wasting or tremors should be present. Note forward thrust when in midline. Ask person to say “light, tight, dynamite,” note lingual speech (sounds of letters l, t, & d is clear and distinct)
Atrophy Tongue deviates to side with lesions of hypoglossal nerve (when this occurs, deviation is toward paralyzed side).
Lobes of the cerebral Frontal o Personality, behavior, intellect & emotions o Broca’s motor speech area- mediates motor speech Expressive aphasia- injury in dominant hemisphere, person cannot talk but can comprehend. Knows what he or she wants to say, but can produce only a garbled sound o Precentral gyrus- initiates voluntary movement
Quadriceps reflex (“knee jerk”) (L2 to L4): Let lower legs dangle freely to flex knee & stretch tendons. Strike tendon directly just below patella. Also, palpate contraction of quads. Alternatively, in supine, use your arm as a lever to support leg against other leg. Normal: extension of lower leg Achilles reflex (“ankle jerk”) (L5 to S2): Position person w/knee flexed & hip externally rotated. Hold foot in dorsiflexion, strike Achilles tendon directly Alternatively, supine, flex one knee & support that lower leg against the other so it falls “open”. Dorsiflex foot, tap tendon Normal: foot plantar flexes against your hand Clonus: Test when reflexes are hyperactive. Support lower leg in one hand, with other hand move foot up & down a few times to relax muscle, stretch muscle by briskly dorsiflexing foot. Hold stretch. Normal: no further movement
ABNORMAL in adults: Babinski Sign- Stoke lateral edge of foot= fanning toes Disappears after age 2- 2. Suck Reflex Touch lips = strong sucking reflex Disappears after 10-12 months Palmer Grasp Reflex Offer finger from ulnar side- symmetrical grasp Present at birth- disappears at 3-4 months Plantar Grasp: thumb to ball of foot- toes curl down disappears after 10 months
Clonus- repeated reflex muscular movements. Hyperactive reflex w/ sustained clonus (lasting as long as the stretch is held) occurs w/ upper motor neuron disease 1) You will feel & see rapid, rhythmic contactions of calf muscle & movement of foot
Reflex Arcs- Involuntary, act under unconscious control and acting quick to potentially painful or damaging situations. Also helps the body maintain balance and appropriate muscle tone 4 types of reflexes: o Deep tendon reflex (myotatic, ex: knee jerk) 5 components: Intact sensory nerve (afferent) Functional synapse in the cord Intact motor nerve fiber (efferent) Neuromuscular junction Competent muscle If one component does not work, there is no reflex. “All or nothing”. o Superficial (corneal reflex, abdominal reflex) o Visceral (organic)- CN III – pupillary response to light & accommodation o Pathologic (abnormal)- ex: Babinski (or extensor plantar) reflex
Subjective data Past history of head injury (location, LOC)? Do you have frequent or severe headaches?
o Patient who says, “this is the worst headache of my life” is an emergency. Referral to screen cerebrovascular cause. Any dizziness or vertigo? o Dizzinesss- light-headed, you or the room is not moving o Vertigo- rotational spinning caused by neurologic disease in vestibular apparatus in the ear or in the vestibular nuclei in the brainstem Objective vertigo- feel as the room is spinning Subjective vertigo- feel as you are spinning Syncope? Sudden loss of strength, a temporary loss of consciousness (a faint), due to lack of cerebral blood flow (low BP) Tremors? (Hands or face) is an involuntary shaking, vibrating, or trembling Weakness? Paresis- partial or incomplete paralysis History/present seizures? o Seizures- occurs w/ epilepsy, a paroxysmal disease characterized by altered or loss of consciousness, involuntary muscle movements, and sensory disturbances o Aura- (warning sign) subjective sensation that precedes seizure; could be auditory, visual, motor Any difficulty swallowing? Any difficulty speaking? o Dysarthria- difficulty forming words o Dysphasia- difficulty w/ language comprehension or expression Do you have any coordination problems? o Dysmetria- inability to control the distance, power, and speed, of a muscular action (balance, clumsy, falling) Do you have any numbness or tingling? o Paresthesia- an abnormal sensation ( burning, tingling) Do you have any significant past neurological history? Are you exposed to any environmental or occupational hazards? o Review anticonvulsants (treatment for seizures), anti-tremor, anti-vertigo, pain medication Additional information: Older adult Any decrease in memory or change in mental functioning? o Memory loss and cognitive decline are early indicators of Alzheimer disease and can be mistaken for normal cognitive decline of aging Any tremors in the hands or face? o Senile tremor is relieved by alcohol (not recommended treatment). Asses if abusing alcohol. Any sudden vision changes? Any sudden weakness on one side of the body and not the other? Ever experience loss of consciousness? o Screen symptoms for stroke
Objective Data Neurological Exam Screening o seemingly well persons with no significant subjective findings from history Complete o who have neurologic concerns (Headache, weakness, loss of coordination) or show signs of neurologic dysfunction o sequence for the complete neurological examination:
- Mental status
- CN
- Motor system
- Sensory system
- Reflexes Neurologic Re-Check o Deficits o Require Periodic Assessments (hospitalized persons or those in extended care)
Health Assessment Final Review
Course: Foundations Of Health Assessment (NUR 3029)
University: Nova Southeastern University
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades

This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades