- Information
- AI Chat
Asthma case study
Pediatrics Nursing Lab (Nur 112)
Pennsylvania College of Health Sciences
Preview text
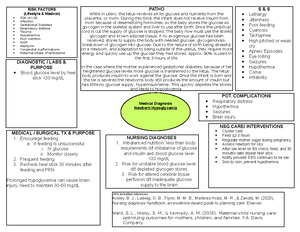
Pediatric Asthma
UNFOLDING Reasoning
Jared Johnson, 10 years old
Primary Concept
Gas Exchange
Interrelated Concepts (In order of emphasis)
- Inflammation
- Clinical Judgment
- Patient Education
- Communication
- Collaboration
UNFOLDING Reasoning Case Study: STUDENT
Pediatric Asthma
History of Present Problem:
Jared Johnson is a 10 year-old African-American boy with a history of moderate persistent asthma. He is being admitted to the pediatric unit of the hospital from the walk-in clinic with an acute asthma exacerbation. Jared started complaining of increased chest tightness and shortness of breath one day prior to admission. He has been at 50 percent of his personal best measurement for his peak expiratory flow (PEF) meter reading which did not improve with the use of albuterol metered dose inhaler (MDI) (per his written asthma management plan). In the walk-in clinic Jared is alert, speaking in short sentences due to breathlessness at rest. He has coarse expiratory wheezes throughout both lung fields with decreased breath sounds at the right base. His oxygen saturation on room air is 90%. His color is ashen and he has dark circles under his eyes. He is sitting upright and using his accessory chest muscles to breath and has moderate intercostal and substernal retractions. He is complaining of tightness in his chest. Jared was diagnosed with asthma at age 6 years and has three prior hospitalizations for asthma with one admission to the pediatric intensive care unit. He has never had to be intubated with these episodes.
Personal/Social History:
He is accompanied by his mother and 16-year-old sister. Jared lives with his mother, maternal grandmother, and sister in an older housing development in the inner city. He is in the 5th grade and a good student despite two to three absences per school year for his asthma. He likes to ride his bike and is the goalie on the soccer team. He says that he has lots of friends at school and likes his teacher, Mr. Bates, who is also his soccer coach. Both Jared and his mother deny tobacco smoke at home.
What data from the histories are important and RELEVANT; therefore it has clinical significance to the nurse? RELEVANT Data from Present Problem: Clinical Significance:
RELEVANT Data from Social History: Clinical Significance:
What is the RELATIONSHIP of your patient’s past medical history (PMH) and current meds? (Which medication treats which condition? Draw lines to connect.) PMH: Home Meds: Pharm. Classification: Expected Outcome: Moderate persistent asthma
Fluticasone/Salmeterol DPI 100 mcg/50 mcg 1 inhalation bid
Albuterol HFA inhaler 2 puffs every 4-6 hours as needed for symptoms
Montelukast 5 mg every evening at bedtime
- Complaining of SOB and chest tightness 1 day prior to admission.
- 50% of best for peak flow with no improvement after albuterol inhaler and 90% O2 on RA
- Coarse expiratory wheezing bilateral lung fields with decreased breath sounds at R base of lung
- Use of accessory muscles with intercostal/substernal retractions
1) Experiencing physical symptoms related to asthma
2) Showing decreased lung function and pt is not getting
oxygen properly
3) Patient's airway is restricted
4) Patient's body is working harder than necessary to get
oxygen to lungs
1)Lives in older housing development,
inner city.
2)Rides bike and goalie on soccer
team.
1) Possible pollution air bad for asthma and contributes to
exacerbation
2) Physical activity could help inlammation over time,
patient should continue being active.
Cardiac Telemetry Strip:
Interpretation:
Clinical Significance:
Radiology Reports:
What diagnostic results are RELEVANT and must be interpreted as clinically significant by the nurse?
RELEVANT Results: Clinical Significance:
Chest X-Ray (frontal
and lateral views):
hyper-expansion of
airways with otherwise
clear lung fields
Lab Results:
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
RELEVANT Lab(s): Clinical Significance:
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
RELEVANT Lab(s): Clinical Significance:
Complete Blood Count: Current: High/Low/WNL? WBC (4–11 mm 3) 10. Neutrophil % (42–72) 55 Hgb (12–16 g/dL) 14. Platelets (150-450 x10 3 /μl) 350
Basic Metabolic Panel: Current: High/Low/WNL? Sodium (135–145 mEq/L) 138 Potassium (3–5 mEq/L) 3. Glucose (70–110 mg/dL) 80 Creatinine (0–1 mg/dL) 0.
Hyper-expansion shows that the patient is not exhaling appropriately and is keeping in more oxygen in than he can get out. This can lead to too much old oxygen and not enough new oxygen which eventually leaves the patient needing oxygen and possible build of carbon dioxide leading to acidosis.
WNL WNL WNL WNL
N/A N/A
WNL WNL WNL WNL
N/A N/A
Lab Planning: Creating a Plan of Care with a PRIORITY Lab:
Lab: Normal Value:
Clinical Significance: Nursing Assessments/Interventions Required:
End tidal CO
Value: 30 mmHg
nullClinical Reasoning Begins...
1. What is the primary problem your patient is most likely presenting?
2. What is the underlying cause/pathophysiology of this primary problem? (Relate initial manifestations to the pathophysiology of the primary problem) Pathophysiology of Primary Problem: Rationale for Manifestations:
Collaborative Care: Medical Management
Care Provider Orders: Rationale: Expected Outcome: Vital signs every 1 hour and as needed
Continuous oxygen saturation monitoring
Continuous end tidal CO monitoring
Start peripheral IV then saline lock
O2 to keep saturations >93%
Albuterol 2 mg and ipratropium bromide 0 5
35-45 mmHg Low end tital of
CO2 shows that the
patient is not getting
rid of enough
Carbon Dioxide
1) Keep patient in upright position
2) Start patient on oxygen supplement
3) Monitor oxygen saturation
4) Monitor PEF
5) Monitor respirations
6) Seek order for steroid
7) Seek ABG if patient does not begin to
improve
Acute asthma exacerbation Patient is having difficulty bringing in as well
as removing oxygen and CO2, both of which
are dangerou and need to be attended to.
Patient's asthma is causing the restriction of
his airways which is leading to the patient
being unable to breath properly.
1)Can watch for improvement or any changes in vital signs (good or bad)
2)Helps to be sure we are maintaining good oxygen supplement to the patient
3)Watch for any changes or improvement. Allows us to keep an eye out for any acidotic manifestations as well due to access CO2 build up
4)Help maintain fluid for the patient and allow quick access in case that is needed
5)Help patient's oxygen improve and relieve anxiety/distress
6)Help with inflammation and allow the patient to bring in and exhale correctly
1)Temperature will improve with interventions and respirations will go down 2)Get patient's oxygen levels to increase with methylprednisone 3)Can watch for any changes that may lead to acidosis 4)Help hydrate the patient and keep easy access for emergency medications 5)improvement with patient's overall appearance and improve respiratory distress 6)Saturation improvement and lung sound improvement 7) Improvement of wheezing, respiratory distress, anxiety, oxygen and chest tightness
Patient is not exhailing properly which is causing build up of excess carbon dioxide, and
hyperinflation of lungs which makes it hard for the patient to bring in new, clean oxygen.
Collaborative Care: Nursing
3. What nursing priority (ies) will guide your plan of care? (if more than one-list in order of PRIORITY)
4. What interventions will you initiate based on this priority? Nursing Interventions: Rationale: Expected Outcome:
5. What body system(s) will you assess most thoroughly based on the primary/priority concern?
6. What is the worst possible/most likely complication to anticipate?
7. What nursing assessments will identify this complication EARLY if it develops?
8. What nursing interventions will you initiate if this complication develops?
9. If the worst possible/most likely complication was recognized by the nurse, when would you decide to notify rapid response team to evaluate further?
10. What psychosocial needs will this patient and/or family likely have that will need to be addressed?
11. How can the nurse address these psychosocial needs?
Improving patient's oxygen and asthma exacerbation will help improve the other symptoms
the patient is experiencing
After reassessing patient's plan of care
Reasses the dose of steroid patient is placed on and increase oxygen
Beliefs, culture, and wishes for the patient
Explain the situation to the patient's family and ask if there is anything they want
implemented in his care that represents their beliefs or cultural background.
Lung and cardiac system
Lung assessment and monitoring of vital signs with the continous oxygen monitoring.
Patient needs to be intubated and does not show improvement with implemented care.
Begins showing signs of acidosis.
Evaluation:
Jared has received a total of two albuterol 2 mg and ipratropium bromide 0 mg inhalation
treatments. He was placed on O2 per n/c to maintain O2 sat >93%. His peripheral IV was
established and he received methylprednisolone 72 mg IV.
1 hour later...
1. What data is RELEVANT and must be interpreted as clinically significant by the nurse? RELEVANT VS Data: Clinical Significance:
RELEVANT Assessment Data: Clinical Significance:
Current VS: Most Recent: Current
PQRST:
T: 99 F/37 C (oral) T: 99 F/37 C (oral) P rovoking/
Palliative:
Talking too much provokes
P: 90 (reg) P: 120 ( reg) Q uality: Tightness is better
R: 24 (reg) R: 30 (reg) R egion/Ra
diation:
Anterior chest
BP: 122/70 BP: 114/78 S everity: 2/
O2 sat: 94% 2 liters n/c O2 sat: 90% on room air T iming: Intermittent
End Tidal CO2: 35 End Tidal CO2: 30
Current Assessment:
GENERAL
APPEARANCE:
Resting comfortably, appears in no acute distress, sitting comfortably in high
Fowler’s position
RESP: Breath sounds have mild expiratory wheezing with equal aeration bilaterally, mild
intercostal retractions, able to speak in full sentences with no SOB, chest tightness
has diminished
CARDIAC: Pink, warm & dry, no edema, heart sounds regular with no abnormal beats (sinus
tachycardia), pulses strong, equal with palpation at radial/pedal/post-tibial
landmarks
NEURO: Alert & oriented to person, place, time, and situation (x4), less anxious, but is tired
and wants to nap
GI: Abdomen soft/non-tender, bowel sounds audible per auscultation in all four
quadrants
GU: Voiding without difficulty, urine clear/yellow
SKIN: Skin integrity intact
99 F
90 pulse
24 respiration
94 % O2 with 2L n/c
End tidal volume 35
Shows the patient is able to breath and the body can control
temperature better
Patient is recieving oxygen and is able to deliver oxygen to
the body easier
Patient is no longer in respiratory distress
Resting comfortably, skin pink, warm, dry. Able to speak in full sentences, no SOB and chest tightness diminished. Improvement in breath sounds and intercostal retractions
Shows that the patient is begining to feel better and breathe
without pain or hyperventilation. Patient lungs sound better
which shows that the care implemented is allowing the
patient to head in the right direction.
Education Priorities/Discharge Planning
1. What will be the most important discharge/education priorities you will reinforce with their medical condition to prevent future readmission with the same problem?
2. What are some practical ways you as the nurse can assess the effectiveness of your teaching with this patient?
Caring and the “Art” of Nursing
1. What is the patient likely experiencing/feeling right now in this situation?
2. What can you do to engage yourself with this patient’s experience, and show that he/she matter to you as a person?
Use Reflection to THINK Like a Nurse
Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention in the moment as the events are unfolding to make a correct clinical judgment.
1. What did I learn from this scenario?
2. How can I use what has been learned from this scenario to improve patient care in the future?
Stress, fatigue, anxious and scared.
Follow up that the patient has an appointment
I think patient should follow up with respiratory therapist to develop better asthma
maintence plans and improve breathing hygiene
I learned how to prioritize patient care, how to create a plan to improve patient's current
state and evaluate the outcome of the interventions implemented
I can look at the body as a whole, using all the information provided to me to figure out the
best course of action for the patient. Not just based on their symptoms, labs, etc but also
based on their home life, social history and how they are feeling.
Keep patient involved in care, explain to him everything that is going on as you go along.
Occasionally ask the patient how he is feeling and help the family be active in his care as
well.
Asthma case study
Course: Pediatrics Nursing Lab (Nur 112)
University: Pennsylvania College of Health Sciences

- Discover more from: