- Information
- AI Chat
This is a Premium Document. Some documents on Studocu are Premium. Upgrade to Premium to unlock it.
Was this document helpful?
This is a Premium Document. Some documents on Studocu are Premium. Upgrade to Premium to unlock it.
Health Assessment Skin Condition
Course: Advanced Health Assessment (NURS 6512)
550 Documents
Students shared 550 documents in this course
University: Walden University
Was this document helpful?
This is a preview
Do you want full access? Go Premium and unlock all 10 pages
Access to all documents
Get Unlimited Downloads
Improve your grades
Already Premium?

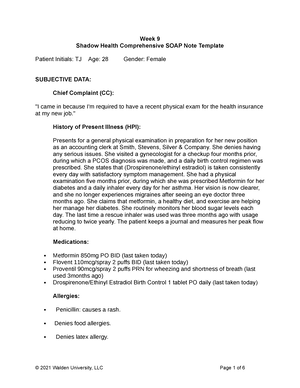
SOAP NOTE
Differential Diagnosis for Skin Conditions
Skin Condition Picture # 5
Patient Initials: __AJ___ Age: __24___
Gender: __F___
SUBJECTIVE DATA:
Chief Complaint (CC): Painful rash and joint pain
History of Present Illness (HPI): Anna James is a 24-year-old
Caucasian female who presents today with a new onset of a painful
plaque-like rash and joint pain 3 weeks ago. She reports she first
noticed the rash on her knees and it has now developed on her
elbows and scalp. She also reports that the rash is sore and slightly
itchy. Anna has also noticed achy joints as well throughout the last
3 weeks. She reports that stressful situations seem to exacerbate
the issue. She has changed laundry detergent and noticed no
improvements in the rash, and she has also been taking Ibuprofen
400mg 3 times a day most days with little relief in pain. Anna
reports the severity of her rash and joint pain to be 6/10.
Medications:
1 Over-the-Counter Ibuprofen 400mg PO every 6 hours as needed
2 Women’s Multivitamin 1 tablet PO daily
3 Ortho Tri-Cyclin 1 tablet PO daily
Allergies: No known drug or food allergies.
Why is this page out of focus?
This is a Premium document. Become Premium to read the whole document.
Why is this page out of focus?
This is a Premium document. Become Premium to read the whole document.
Why is this page out of focus?
This is a Premium document. Become Premium to read the whole document.