- Information
- AI Chat
This is a Premium Document. Some documents on Studocu are Premium. Upgrade to Premium to unlock it.
Was this document helpful?
This is a Premium Document. Some documents on Studocu are Premium. Upgrade to Premium to unlock it.
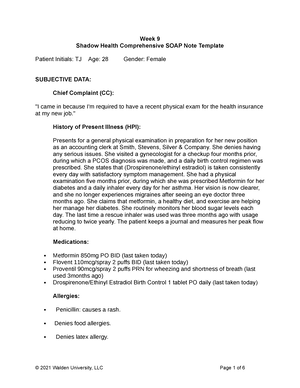
Tina jones comprehensive
Course: Advanced Health Assessment (NURS 6512)
550 Documents
Students shared 550 documents in this course
University: Walden University
Was this document helpful?
This is a preview
Do you want full access? Go Premium and unlock all 7 pages
Access to all documents
Get Unlimited Downloads
Improve your grades
Already Premium?

2/24/2019 Comprehensive Assessment | Completed | Shadow Health
https://app.shadowhealth.com/assignment_attempts/4562098 1/7
Comprehensive Assessment Results | Turned In
Health Assessment for the BSN - Muskegon - Spring 2019, NUR 2250
Return to Assignment
Undergraduate students, become a tester for Shadow Health!
Undergraduate students, become a tester for Shadow Health! Click here for more information
Click here for more information
If you are using Safari and have issues with audio in your assignment, please click here for assistance.
If you are using Safari and have issues with audio in your assignment, please click here for assistance. Click here for more information
Click here for more information
Your Results Lab Pass
Lab Pass
Documentation
Vitals
Student Documentation
Student Documentation Model Documentation
Model Documentation
Vitals
BP: 142/82; HR: 68; RR: 16; O2: 98%; Temperature:
37.9 C
• Height: 170 cm
• Weight: 84 kg
• BMI: 29.0
• Blood Glucose: 100
• RR: 15
• HR: 78
• BP:128 / 82
• Pulse Ox: 99%
• Temperature: 99.0 F
Health History
Student Documentation
Student Documentation Model Documentation
Model Documentation
Identifying Data & Reliability
Patient is in no apparent distress. Alert and oriented
x4. Patient is seated upright on the examination
table, she is well nourished, and dressed
appropriately for the weather with good hygiene.
Ms. Jones is a pleasant, 28-year-old African
American single woman who presents for a pre-
employment physical. She is the primary source of
the history. Ms. Jones offers information freely and
without contradiction. Speech is clear and coherent.
She maintains eye contact throughout the interview.
Overview
Transcript
Subjective Data Collection
Objective Data Collection
Documentation
Plan My Exam
Documentation / Electronic Health Record
https://www.coursehero.com/file/38245035/Comprehensive-Assessment-Completed-Shadow-Healthpdf/
This study resource was
shared via CourseHero.com
Why is this page out of focus?
This is a Premium document. Become Premium to read the whole document.
Why is this page out of focus?
This is a Premium document. Become Premium to read the whole document.