- Information
- AI Chat
Lecture Notes
Health and Healing IV (NURS-3005EL)
Laurentian University
Recommended for you
Related Studylists
community nursingPreview text
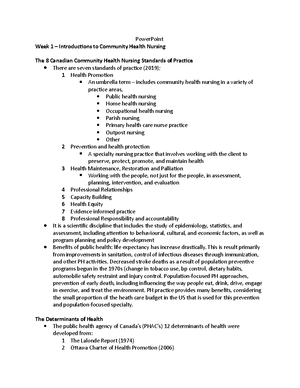
PowerPoint Week 1 – Introductions to Community Health Nursing
The 8 Canadian Community Health Nursing Standards of Practice There are seven standards of practice (2019); 1 Health Promotion An umbrella term – includes community health nursing in a variety of practice areas, Public health nursing Home health nursing Occupational health nursing Parish nursing Primary health care nurse practice Outpost nursing Other 2 Prevention and health protection A specialty nursing practice that involves working with the client to preserve, protect, promote, and maintain health 3 Health Maintenance, Restoration and Palliation Working with the people, not just for the people, in assessment, planning, intervention, and evaluation 4 Professional Relationships 5 Capacity Building 6 Health Equity 7 Evidence informed practice 8 Professional Responsibility and accountability It is a scientific discipline that includes the study of epidemiology, statistics, and assessment, including attention to behavioural, cultural, and economic factors, as well as program planning and policy development Benefits of public health: life expectancy has increase drastically. This is result primarily from improvements in sanitation, control of infectious diseases through immunization, and other PH activities. Decreased stroke deaths as a result of population preventive programs begun in the 1970s (change in tobacco use, bp control, dietary habits, automobile safety restraint and injury control. Population-focused PH approaches, prevention of early death, including influencing the way people eat, drink, drive, engage in exercise, and treat the environment. PH practice provides many benefits, considering the small proportion of the heath care budget in the US that is used for this prevention and population-focused specialty.
The Determinants of Health The public health agency of Canada’s (PHAC’s) 12 determinants of health were developed from: 1 The Lalonde Report (1974) 2 Ottawa Charter of Health Promotion (2006)
3 The Epp Report (1986)
Social Determinants of Health Definition: The economic and social conditions that shape the health of individuals, communities, and jurisdictions as a whole Recent literature points to the importance of social determinants of health for client health
14 Social Determinants of Health 1. Income and income distribution 2. Education 3. Unemployment and job security 4. Employment and working conditions 5. Early childhood development 6. Food insecurity 7. Housing 8. Social exclusion 9. Social safety network 10. Health services 11. Aboriginal status 12. Gender 13. Race 14. Disability
Community health and primary care defined Community health: Meeting collective needs by identifying health concerns and strengths and managing behaviours within the community and between the community and the larger society Primary care: Provides the first contact between individuals and the health care system and usually refers to the curative treatment of disease, rehabilitation, and preventive measures
Primary Health Care In the early 1970s, the most common model used in health care was the medical model, which focused on treatment and cure in institutions In 1974, the Lalonde Report initiated a shift-toward population health promotion In 1978, at the Alma-Ata conference, primary health care became the preferred international strategy Primary health care is: o A model defined as essential health care that is comprehensive and addresses social justice and equity issues o Based on practical, scientifically sound, and acceptable methods and technology o Universally accessible to individuals and families in the community at a cost that the community and country can afford to maintain
Population Health Promotion Approach A population health promotion approach recognizes that health is a capacity or resource and recognizes the range of social, economic and physical environmental factors that contribute to health within a population including the entire range of individual and collective factors and conditions and their interactions that have been shown to be correlated with health status
Health Promotion (Traditional) The focus of all purposeful activities designed to improve personal and public health through a combination or strategies, including o Behavioural change o Health education o Health protection measures o Risk factor detection o Health enhancement o Health maintenance
Primary Care - focus on individual - Individualized clinical services - Secondary & Tertiary disease prevention - Health Education - Examples : - General Practice - Diabetic Clinic - Heart Health Clinic - Screening Programs
Selective Primary Health Care - Population Health through individuals - Screening and surveillance - Immunization - Primary prevention - Health education - Examples: - Healthy Heart Programs - Well child clinics - Flu Clinics
Comprehensive Primary Health Care
- tackles social determinants of health
- Provision of housing, shelter, social support, food and nutrition, safe environments
- Capacity building and health promotion
- Health impact awareness
- Harm minimization approaches
- Advocacy for sustainable social and system change
- Examples:
- Youth Health centers
- Healthy Public Policies
- Food Security work
In community health nursing practice one area of focus = disease prevention at 3 levels o Primary prevention focuses on risk factors and health promotion (seeks to prevent disease from the beginning) ex. Health education o Secondary prevention is used after a stressor has penetrated the community subsystems: Seeks to detect disease early in its progression in order to make early diagnosis and begin treatment. Ex screening
o Tertiary prevention focuses on residual consequences of a stressor’s impact: Begins once a disease has become obvious; aims to interrupt the course of the disease and re-establish equilibrium
Primary Prevention Goal: Reduce number of new cases of a disease Rational: By reducing exposure rates and increasing resistance, can number of new cases. Ex: Chlorinating the city water supply Target population: Those who are likely to be exposed and/or could increase their resistance Typical activities o Remove or reduce source of the risk o Educate and make aware of diseases risk Include behavioural changes to reduce exposure o Improve general health Outcome Measure: Number of exposures to a causative agent or risk factor, final outcome would be number of new cases of disease (incidence) o Incidence = the number of new cases in a given period o Incidence rate= ratio of new cases to total population at risk for a given period of time. Allows comparison of incidence to other disease or other population
Secondary Prevention Goal: Reduce number of new cases; reduce number of severe cases o Reducing the severity of disease (reducing morbidity) and new cases (incidence) are the ultimate goals of secondary prevention. This may apply to the individual cases (reduce severity of symptoms or duration of illness) and the community (reduce severity of outbreak) Rationale: By reducing number of exposures and early disease that progress to more severe disease, mortality and morbidity can be reduced. o Early detection of a disease-causing exposure or identifying a disease in its early stages can lead to early treatment to either stop the progression of the disease or reduce its severity which will reduce complications. Identifying those who are sick can also aid in reducing the spread of the disease to others in the community Target population: Those who have been exposed to the disease-causing agent or have early symptoms of the disease o This now becomes the individuals who were in the ‘risk exposure” or “risk of disease” group who have been exposed or have early disease. So, it is a subset of the primary prevention population for that specific disease Typical activates o Screening for exposure and/or disease o Post-exposure prophylaxis o Early treatment to reduce impact of disease/reverse course
Since ancient times, people have been trying to prevent, understand, and control disease Examples: o Ancient Babylonians: understood need for hygiene; some medical skills o Egyptians: variety of pharmaceutical preparation; public drainage systems; earth privies o Ancient Greeks: concerned with personal health-cleanliness, exercise, diet, & sanitation o Classic Romans: regulation of medical practice; punishment for negligence; visits to the sick o Christianity: brought ideas of personal responsibility for others o Middle Ages: walled-in cities created crowding and poor sanitation o Renaissance: human dignity & worth; Elizabethan Poor Law o Industrial Revolution: previous care structures (family & friends) were not enough so created nursing care institutions & homes
Florence Nightingale 1850s: Sent by the British government to Asia Minor to care for soldiers wounded in the Crimean War Using simple epidemiological measures, documented a mortality rate that decreased from 415 per 1000 at the beginning of the war to 11 1000 at the end of it Returned to England and revamped nursing education, replacing untrained lay nurses with “Nightingale nurses”
William Rathbone 1859: The British philanthropist founded the first association for district nursing o This led to the establishment of district nursing throughout the U o It also led to the establishment of the Victorian Order of Nursing (VON)
Early Public Health Efforts Driven by the need to deal with epidemics Immigrants arrived from Europe carrying highly contagious disease (ex. Smallpox, typhus, cholera, and influenzas Epidemics killed tens of thousands of people, especially Aboriginal peoples Canadians authorities began to take action to protect public health, introducing vaccination programs and establishing boards of health
Early Development of Community Health Nursing in Canada In the early years of North American settlement, the sick was cared for informally in the home, by the women of the household In the seventeenth and eighteenth centuries, these women, religious orders, and wealthy philanthropists took care of the sick who could not afford their own care
Beginnings of Public Health Nursing Early 1900s: o Organized public health nursing became a major component of public health programs o Public health nurses (PHNs) began making home visits to treat TB o Various districts implemented public health nursing programs such as visiting families with newborns, visiting schools, etc.
Eunice Dyke Early 1990s: This Ontario nurse became interested in public health 1911: She became the first director of public health nursing in Toronto Public health nursing evolved in Canada in the late 1900s and early 2000s largely because of her pioneering work
Milestones in Public Health Nursing in Canada In 1917, Manitoba became the first province in Canada to establish a public health nursing service Public health district nurses worked in isolated rural communities where no other medical services were available 1919- o Public health nursing began to focus on screening programs o The Canadian federal government initiated social assistance for health care o Provinces concentrated on public health programs such as immunizations, improved sewage systems, and clean water 1918- o Canadian universities began to offer degree programs o The Weir Report of 1932 concluded that public health nursing should become a specialty area in advanced education
Community Health Nursing Milestones Early 1920s: o A public health nursing practice section of the CNA was formally recognized 1932 o The Weir Report proposed solutions for several important issues in public health nursing practice 1920- o Nurses specializing in TB care were replaced by PHNs
Community Health Nursing from the 1920s to Present Day 1950-1960s o PHNs became generalists, visiting clients in homes, schools, and clinics 1970s
o Learners/practitioners seek out, integrate and value, as a partner, the input and engagement of patient/client/family/community in designing and implementing care/services Interprofessional Communication o Learners/practitioners from varying professions communicate with each other in a collaborative, responsive and responsible manner
Week 2 – Working with Groups, Teams and Partners
Working with Groups Groups that CHNs work with o Families o Self-help groups o Community groups o Health care teams o Professional associations o Committees CHNs must consider the following characteristics o The purpose of the group o Group membership o Group dynamics o Group process o Group leadership o Group size o Group task and maintenance functions
Definitions Group: A collection of two or more individuals in face-to-ace interactions with a common purpose and how are in an independent relationship Team: A specialized group working towards a common goal or activity o Types include; interprofessional, intraprofessional, and intersectoral Community-oriented nursing can focus on either the community (population-focused) or on individuals, families and groups Community-based nurses only focus on the individual and families
Group Process Five dimensions of group process to function effectively: o Group physical and emotional climate o Group involvement o Group interaction o Group cohesion o Group productivity
Group Development Tuckman and Jensen’s five stages of group development o Stage 1: Forming: Group members, as strangers, focus on getting to know each other o Stage 2: Storming: Group members begin to express their feelings as they focus on real issues o Stage 3: Norming: Group member start to feel part of the group; they recognize the benefits of the group reaching its goal o Stage 4: Performing: Group members focus on the group work with sharing of ideas in a supportive group environment o Stage 5: Adjourning: Group members recognize the need for termination of the group and therefore work towards completion of the tasks and disengage from other group members
Group Roles Roles that may be assumed by group members as the group develops: o Task roles: Focus on problem solving and decision making o Maintenance roles: Focus on creating a comfortable climate and facilitating group interaction o Non-functional roles: Individual roles in the group that hinder group cohesiveness and productivity
Group Norms Rules and standards that set the stage for how the group will proceed in reference to how decisions are made, how work is assigned, and what acceptable member behaviour is Often follow a standard from of decision making (Ex. Robert’s Rules of Order)
Group Leadership Refers to influencing and directing others Includes acts that assist the group in meeting its goal(s) and influence group actions to maintain the group Strong leadership is essential for groups to function effectively
Leadership Styles most often used Autocratic – Authoritarian or paternalistic work; work demands and not work requests are made; decision making does not involve others; best used when decisions need to be made quickly; can help reduce member frustration Laissez-faire- Non-directed delegative style, leader assumes little or no group control, minimal direction, shared decision making, works for problem solving where no tight time constraints Democratic/participative – Leader has some group control, group members involved in decision making when thorough problem solving required; is time consuming
o Compromising – members explore solutions and negotiate a solution that is equal for all members o Accommodating – members cooperate and give in to other members for benefit of group o Collaborating – members examine differences that exist and work together to establish acceptable solution that is beneficial to all group members
Effective Team Building Goal is to develop highly efficient teams that demonstrate o Participative leadership – consult with team members o Shared responsibility – all members responsible o Aligned on a purpose – team shares same goal o Strong communication – openness, respect, trust, honesty o Future focused – Professional & personal growth expected o Focused on task – Stays on task to achieve results o Creative talents – Member talents encouraged & applied o Rapid response – Possibilities recognize and acted on ASAP
Interprofessional Partnerships Attributes of effective interprofessional partnership include o Each partner recognizes the purpose and need for the partnership o A collegial relationship is valued o Interdependency exists among partner members o Power and leadership are shared by the partners Collaborative client-centred practice: o The active involvement of health care professionals from various disciplines in working together collaboratively to improve client health outcomes o This model of health care practice facilitates improvement of population health, client health, access to health are, communication among, health care professionals, and better utilization of human health care resources
Week 3 – CHNs Practice in Canada: Standards & Competencies
What is a Code of Ethics? The CAN code of Ethics for RNs is a statement of the ethical values of RNs and nurses licensed in extended roles. Ex. Nurse practitioners. It demonstrates nurses’ commitment to persons with health-care needs and persons receiving care. It is for all nurses Ex. In clinical practice, education, administration, research or policy Ethical Foundations of Public Health and Community Practice Inclusion Diversity Participation Empowerment
Social Justice Advocacy Interdependence
Ethical Challenges of CHNs Respecting individual autonomy vs protecting the community Goals of social justice and empowerment can be difficult to achieve Facilitation and ensuring inclusion and diversity Establishing appropriate client boundaries
Difference between standards & competencies Standards: Define the scope and depth of practice by establishing criteria for acceptable nursing practice Competencies: Are the integrated knowledge, skills, judgment and attributes required of a RN to practice safely and ethically. Attributes include attitudes, values and beliefs
Importance of CCHN Standards Define scope and depth of CHN practice Establish criteria and expectations for acceptable practice and safe ethical care Provide criteria for measuring performance Support the ongoing development of CHN Promote CNH as a specialty and provide a foundation for certification as a clinical specialty with CNA Inspire excellence in & commitment to CHN practice Set a benchmark for new community health nurses
Standard 1: Health Promotion Involves the population as a whole in the context of their everyday life rather than focusing only on at-risk people The process of addressing health inequities and enabling people to increase control over & to improve their health Brings together people who recognize that basic resources & conditions for health are critical (Social and environmental determinants of health) Works best when all levels-individuals, groups, community, society (government, media) and multiple approaches are used Practice examples: o PHNs work with a community to advocate for a smoke-free town or municipality o PHNs promote physical activity and healthy eating through programs such as the In-motion, supermarket safari and the school’s awards program o HHNs encourage families dealing with a chronic illness to participate in regular physical and social activities
Standard 2: Prevention & Health Protection
Capacity building describes an increase in ability of individuals/ communities to define, assess, analyze & act on health concerns Active involvement by those affected is critical CHN works collaboratively with those affected by the health concern and those who control resources CHNs assess the stage of readiness for change & priorities for action CHNs build on existing strengths In comparison to institutional practice with individuals, CHNs build capacity at the group, organization and community level CHN build on existing strengths 0 this may include seeking organizational elements which represent the ways in which people come together in order to socialize and address their concerns. These organizational structures may include small group such as committees, church and youth groups Practice Ex. o An HHN encourages a mother and teens to work out a schedule for ROM exercises for the grandmother. The family is happy that they were able to work out the problem together o A PHN encourages a school to mobilize a school health committee that includes students, parents, teachers, administrations, and community partners. Committee members identify the school community’s strengths and needs, and prioritize, plan, implement, evaluate and celebrate action for a healthier school. The school community’s capacity to take its own action for health is enhanced via a sustainable structure (the committee). The PHN is a partner is the process
Standard 6: Health Equity CHNs identify & facilitate universal & equitable access to services and recourses CHNs engage in advocacy on many levels including services appropriate for cultural groups in the community CHNs collaborate with other services and sectors to promote effective working relationships that contribute to comprehensive client care & achievement of optimal outcomes This standard is particularly unique to CHNs. CHNs bring health care to people where they live, work, play, learn, workshop. This includes on the streets, in their homes and in community meetings CHN engage in advocacy by analyzing the full range of possibilities for action, acting on affected determinants of health & influencing other sectors to ensure their policies & programs have a positive impact on health Practice Ex. o A PHN identifies that one ethic group does not use health care services (including prenatal classes) outside their area. The PHN works with a champion from this group to organize local prenatal classes delivered by a PHN and translated by a woman from the community (CHNAC) o A HHN and case manager advocate for families caring for medically fragile children by
Seeking respite care for an exhausted family Contracting the local MPP Planning for a resolution through Provincial/Territorial nursing association
Standard 7: Evidence-Informed Practice The community health nurse consults the research literature and Health Canada in order to provide competent care Ex. Uses Canada food guide use when teaching about nutrition
Standard 8: Professional Responsibility & Accountability CHNs work with a high degree of autonomy – accountable for their competency & quality of their practice CHNs work in a complex environment with accountability to a variety of authorities CHNs encounter unique ethical dilemmas The complex environment in which CHN work and the high degree of autonomy they have makes this standard more challenging CHN are responsible not only for nursing care of individuals, but also for the health of communities and populations. CHN work with many organizations, governmental levels and businesses Unique ethical dilemmas are encountered These include whether responsibility for an issue lies with the individual/community/population or with the nurse or the nurse’s employer Practice Ex. o A HHN is asked by an ALS client to be present when his wife removes his Bi-PAP machine, which will result in his death. The nurse explores the client’s reason for this decision and discusses the ethics around responding to this request with the health care team as well as the nursing practice advisor at the College of Nurses o A PHN is assigned to work in a needle exchange program based on harm reduction. He has difficulty accepting the tenets of harm reduction and uses reflective practice personally and with his supervisor to understand and change his assumptions o Both teamwork and communication are reduced after the hiring of a new manager. You have been with the program for a while and can see that people are not receiving the same level of services and newly hired staff are not being supported. You decide to meet with the new manager to discuss the situation. Depending on the response from the manager, you will either go to a higher level or offer to collaborate to improve the work and service environment
Entry -to- Practice Public Health Nursing Competencies for Undergraduate Nursing Education Domain 1: Public health sciences in Nursing Practice Domain 2: Population and Community Health Assessment and Analysis Domain 3: Population Health Planning, Implementation, and Evaluation
Role in Disease and Injury Prevention : Ex. Applies epidemiological principles and knowledge of the disease process so as to manage and control communicable diseases using prevention techniques, infection control, behaviour change counselling, outbreak management, surveillance, immunization, episodic care, health education, and case management Role in Health Protection : Ex. Acts in partnership with public health colleagues, government, and other agencies to: o Ensure sage water, air, and food, o Control infectious diseases, and o Provide protection from environmental threats Role in Health Surveillance: Ex. Mobilizes formal and/or informal networks to systematically and routinely collect and report health data for tracking and forecasting health events or health determinants Role in Population Health Assessment: Ex. Plays a key role in producing and using knowledge about the health of communities (or certain populations or aggregates) and the factors that support good health or pose potential risks (determinants of health), to produce better policies and services Role in Emergency Preparedness and Response: Ex. Plans for, is part of, and evaluates the response to both natural disaster (such as floods, earthquakes, fires, or infection diseases outbreaks) and man-made disasters (such as those involving explosives, chemicals, radioactive substances, or biological threats) to minimize serious illness, death, and social disruption
Week 4: Community Health Assessment 1: Asset Mapping and Windshield Survey
Community Health A broad Definition: o Community health is the process of involving the community in maintaining, improving, promoting, and protecting its own health and well-being o This definition emphasizes the process dimension but also includes the dimensions of status and structure
Community Persons who interact and have similar goals or interests and share common social supports, and may or may not come within the same geographic boundaries A locality-based entity composed of systems of formal organizations reflecting society’s institutions, informal groups, and aggregates (groups within a population)
Types/Kinds of Communities Community of interest: Hiking club Community of concern: Ex high STI rate Neighbourhood community: ex. Geography Community of practice: PHNs for nutrition
Community Health Dimensions The concept of community health has three common dimensions 1) Status 2) Structure 3) Process
Dimension of Community Health Status: o Often measured by: Traditional morbidity and mortality rates Life expectancy indices Risk factor profiles o Structure: Includes community health services and resources and attributes of the community structure itself, commonly identified as social indicators or correlates of health o Process Community health is the process of effective community functioning or problem solving
Healthy Communities Healthy cities/healthy communities o In the mid 1980s, the world health organization (WHO) began an international initiative promoting healthy communities in Europe o The terms healthy cities movement and healthy communities’ movement are used interchangeably o This movement incorporates the primary health care principle of health promotion in order to achieve “health for all” and includes more than 7500 cities and towns worldwide o “A healthy community is one where people, organizations and local institutions work, together to improve the social, economic and environmental conditions that make people healthy – the determinants of health Community-as-partner Model A partnership conveys an egalitarian relationship between the CHN and the community Vollman suggests that people in the community are the CHN’s partners and need to be included during the entire community health nursing process
Effective Communities Look inside first to solve problems Have good sense of assets, capacities and needs Leaders open doors Citizens are involved People take responsibility
Lecture Notes
Course: Health and Healing IV (NURS-3005EL)
University: Laurentian University

- Discover more from: