- Information
- AI Chat
Patient Research - Schizophrenia
Nursing Practice Mental Health Nursing (Nurs 279)
MacEwan University
Preview text
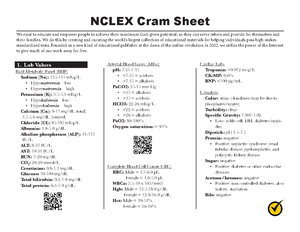
Shadow Health Scenario: Schizophrenia Patient Name: Eric Ford Psychiatric Diagnoses: Paranoid chronic with acute exacerbation Mental disorder in which there exists disturbances in thought content and form, perception, affect, language, social activity, sense of self, volition, interpersonal relationships, and psychomotor behavior Can progress to social withdrawal, perceptual distortions, chronic delusions, and hallucinations May result in only one psychotic episode for up to of patients For some patients, may result in no disability between periods of exacerbation, whereas other patients may need continuous institutional care o Worsening prognosis with each acute episode A biochemical hypothesis holds that schizophrenia results from excessive activity at dopaminergic synapses, leading to active psychotic signs and a decrease in prefrontal activity of dopaminergic pathways leads to negative and cognitive symptoms. o Other neurotransmitter alterations may also contribute to schizophrenic signs and symptoms, such as norepinephrine, serotonin, glutamate neurotransmission involving the receptor, and acid transmission. Structural abnormalities of the intraventricular system, temporal lobe abnormalities, decreased volume of the amygdala and hippocampus of the limbic system, structural changes in prefrontal white matter, and increased volume of the basal ganglia have been found. o Altered brain structure and function may also result from overactivity of the immune system. Causes: exact cause is unknown, but it may result from a combination of genetic, biological, cultural, and psychological factors Risk factors: family history of schizophrenia, maternal malnourishment or viral illness during pregnancy Symptoms: o Positive Signs Symptoms: Delusions (grandiose, nihilistic, paranoid, erotomanic) Hallucinations Disjointed, disconnected speech patterns (tangentiality, circumstantiality, derailment, neologisms, word salad) Disorganized behaviour (aggression, agitation, catatonic excitement, echopraxia, regressed behaviour, stereotyped behaviours, hypervigilance, waxy flexibility) o Negative Signs Symptoms: Flat affect Ambivalence Difficulty with emotional expression Anhedonia (little interest in social activities or relationships) Alogia (limited speech, latent responses) Apathy (poor grooming, failure of role responsibilities) o Cognitive Signs Symptoms: Memory deficits Attention deficits Diminished executive functioning (using information to make appropriate decisions) o Mood Signs Symptoms Depression Anxiety Mood or behaviour that is to understand Complications: suicide, trauma, comorbid substance abuse problems, tardive dyskinesia (due to medications) Diagnostic Criteria (diagnosis depends on identifying two or more of the following signs and symptoms for a significant portion of time during a period), computed tomography scanning (brain), or magnetic resonance imaging (for patients who display abnormal neurologic findings rule out intracranial pathology), electroencephalography (rules out seizure disorder), neuropsychiatric testing may reveal difficulty with processing information, impaired memory, and easy distractibility. Treatment: antipsychotics (neuroleptic drugs), atypical antipsychotics, IM antipsychotics (if adherence to oral agents is poor), benzodiazepines (as adjuncts during acute phase or if patient fails to respond to one or two doses of an antipsychotic agent for agitation), anticonvulsants (adjuncts for agitation or violent behavior), benztropine mesylate (treatment for parkinsonism associated with antipsychotic use) Nursing Administer prescribed ensure that the patient has swallowed the drug and is not it. Evaluate the ability to carry out activities of daily provide assistance as necessary, encourage the patient to participate in care as much as if necessary, break down tasks into simple steps that the patient can avoid promoting dependence. Maintain a safe environment, minimizing stimuli. Institute suicide precautions and develop a safety plan with the patient that includes a list of appropriate coping strategies and sources of support. Remove all potentially harmful items from the observe for changes in behavior that may signal an increasing risk for violence, such as irritability, intimidating behavior, motor restlessness, loud speech, or overt threats. Implement the environment for the patient. Approach the patient calmly and quietly from the speak in a clear, calm, unhurried adopt an accepting and consistent approach. Reward positive behavior. Provide explanations for distorted body image or hypochondriacal complaints. argue with the patient about whether hallucinations are clarify that you perceive the stimuli as the patient does. Focus on the feeling about the delusion rather than on its reinforce the engage the patient in activities and interactions. Set limits on inappropriate behavior. Offer simple and explanations for environmental safeguards, drugs, and policies. Build be honest and dependable. threaten, and promise what you fulfill. Evaluate how the current illness will impact the independence. Identify the formal and informal supports. Identify the and goals, preferences, comprehension, and concerns about discharge. Confirm arrangements for transportation to initial Provide a list of prescribed drugs, including the dosage, prescribed time schedule, and adverse reactions to report to the practitioner. Provide the patient (and family or caregiver, as needed) with written information on the medications that the patient should take after discharge. Assess the and understanding of the prescribed medication, including dosage, administration, expected results, Goals of Care Designation GOC: R1 o Patient is going get all available treatments, including attempted resuscitation and ICU care. Transferring the patient, life support interventions, life sustaining measures, and major surgery are all included. LAB VALUES CBC o evaluate the cells that circulate in blood, including red blood cells (RBCs), white blood cells (WBCs), and platelets (PLTs). The CBC can evaluate her overall health and detect any potential infections or deficiencies (eg. anemia). Urinalysis o detect measure several substances in the urine, such as products of normal and abnormal metabolism, cells, cellular fragments, and bacteria (eg. UTI) Toxicology Screen o checks for drugs or other chemicals in blood, urine or saliva. It may check for one or for up to 30 drugs at once. These may include medicines, nonprescription medicines, vitamins, supplements, alcohol alcohol drugs. Lipid Panel o it looks at total cholesterol, lipoprotein cholesterol lipoprotein cholesterol and triglycerides. Mantoux o used to determine if the patient is infected with mycobacterium tuberculosis. Rapid Plasma Reagin o is a screening test for syphilis measuring detecting nonspecific antibodies. Metabolic Panel (CMP) o provides important information about the current status of the metabolism. It looks at glucose, calcium, albumin, total protein, sodium, potassium, bicarbonate (total CO2), chloride, blood urea nitrogen (BUN), creatinine, alkaline phosphatase (ALP), alanine amino transferase (ALT, SGPT), aspartate amino transferase (AST, SGOT), and bilirubin DIAGNOSTIC TESTING 12 Lead ECG o representation of the electrical activity recorded from electrodes on the body surface. Mental Health Act Certified under the Mental Health Act Medication Research: Home Medications RisperDAL 2mg PO BID o Other names: risperiDONE, Risperdal Consta, RisperDAL o Therapeutic Class: antipsychotics, mood stabilizers o Pharmacologic Class: benzisoxazoles o Indication: schizophrenia, bipolar I disorder, irritability associated with autistic disorder o o o o o o in children Why is this patient using this medication? Patient has schizophrenia. Mechanism of Action: may act antagonizing dopamine and serotonin in the CNS which results in decreased symptoms of psychoses, bipolar mania or autism. Site of Metabolism: extensively metabolized the liver. Contraindications: hypersensitivity or in mothers that are breast feeding as drug can be passed through breast milk Adverse Effects: neuroleptic malignant syndrome, suicidal thoughts, aggressive behaviour, dizziness, extrapyramidal reactions, headache, increase dreams, increase sleep duration, insomnia, sedation, fatigue, impaired temperature regulation, nervousness, tardive dyskinesia, pharyngitis, rhinitis, visual disturbances, cough, dyspnea, arrythmias, orthostatic hypotension, tachycardia, constipation, diarrhea, dry mouth, nausea, weight gain, abdominal pain, anorexia, dyspepsia, polydipsia, increase salivation, vomiting, weight loss, decreased libido, difficulty urinating, polyuria, priapism, rash, dry skin, increased pigmentation, sweating, photosensitivity, seborrhea, dyslipidemia, galactorrhea, hyperglycemia, agranulocytosis, leukopenia, neutropenia, anaphylaxis, angioedema Neuroleptic Malignant Syndrome symptoms: high fever, irregular pulse, tachycardia, tachypnea, muscle rigidity, altered mental status, autonomic nervous system dysfunction resulting in high or low blood pressure, profuse perspiration, and excessive sweating Nursing monitor mental status (orientation, mood, behaviour) and mood before and periodically during therapy monitor closely for notable changes in behaviour that could indicate the emergence or worsening of suicidal thoughts or behaviour of depression especially during early therapy. Monitor patient for onset of extrapyramidal effects (akathisia, restlessness, dystonia, muscle spasms and twisting motions or face, rigidity, tremors, drooling, shuffling gait, dysphagia) monitor for tardive dyskinesia (involuntary rhythmic Inpatient Medication Orders: Nicotine patch hours 1 patch daily o Other names: Nicoderm CQ o Therapeutic Class: smoking deterrents smoking cessation aids o Pharmacologic Class: nicotinic agonists o Indication: adjunct therapy (with behaviour modification) in the management of o o o o o o o nicotine withdrawal in patients desiring to give up cigarette smoking Why is this patient using this medication? Patient is trying to stop smoking. Mechanism of Action: provides a source of nicotine during controlled withdrawal from cigarette smoking Site of Metabolism: mostly metabolized liver, small amounts are metabolized kidneys and lungs 4 hour Contraindications: hypersensitivity or allergy to nicotine, use patch cautiously in patients with skin problems and in those allergic to adhesive tape, use cautiously in patients with diabetes, hyperthyroidism, pheochromocytoma, or severe renal or hepatic impairment, use cautiously in patients with oropharyngeal inflammation, history of esophagitis, or peptic ulcer disease because healing of GI disorders may be delayed Adverse Effects: headache, insomnia, abnormal dreams, dizziness, drowsiness, impaired concentration, nervousness, seizures, weakness, tachycardia, chest pain, hypertension, increase in appetite, increase in salivation, oral injury, sore mouth, burning at patch site, erythema, pruritus, cutaneous hypersensitivity, rash, sweating, dysmenorrhea, allergy, paresthesia Nursing Assess patient for symptoms of smoking withdrawal (irritability, drowsiness, fatigue, headache, nicotine craving) periodically during nicotine replacement therapy. Evaluate progress in smoking cessation periodically during therapy. Instruct patient in application and use of patch. Apply to clean, dry skin of upper arm or torso free of oil, hair, scars, cuts, burns, or irritation. Wash hands with soap and water after handling patches. Do not trim or cut patch. No more than 1 patch should be worn at time. Alternate application sites. Advise that redness, itching and burning at application site usually subside within 1 hr. May cause drowsiness or dizziness caution patient to avoid driving or other activities requiring alertness until response to medication is known. Lorazepam 1mg PO PRN Q4H PRN o Other names: Ativan o Therapeutic Class: anesthetic adjuncts, antianxiety agents, o Pharmacologic Class: benzodiazepines o Indication: anxiety disorder, IM, IV status epilepticus, preanesthetic to produce o o o o o o o o sedation, decrease preoperative anxiety and induce amnesia Why is this patient using this medication? For anxiety agitation Mechanism of Action: Depresses the CNS, probably potentiating GABA, an inhibitory neurotransmitter Site of Metabolism: highly metabolized the liver hr Contraindications: hypersensitivity, with other benzodiazepines may exist, comatose patients or those with CNS depression, uncontrolled severe pain, glaucoma, severe hypotension, sleep apnea, OB, lactation (use in pregnancy and lactation may cause CNS depression, flaccidity, feeding difficulties, hypothermia, seizures, and respiratory problems in the discontinue drug or bottle fed) Adverse Effects: dizziness, drowsiness, lethargy, hangover, headache, slurred speech, forgetfulness, confusion, mental depression, blurred vision, respiratory depression, constipation, diarrhea, nausea, vomiting, weight gain, rashes, physical dependence, psychological dependence, tolerance Nursing conduct regular assessment of continued need for treatment. Prolonged therapy may lead to psychological or physical dependence. Instruct patient to take medication exactly as directed and not to skip or double up on missed doses. May cause drowsiness or dizziness avoid driving or other activities requiring alertness until response to medication is known. Caution patient to avoid taking alcohol or other CNS depressants concurrently with this medication. Teach other methods to decrease anxiety, such as increased exercise, support groups, relaxation techniques. Emphasize that psychotherapy is beneficial in addressing the source of anxiety and improving coping skills. Required Lab Monitoring Frequency of Testing: Patients on therapy should receive routine evaluation of renal, hepatic and hematologic function Haloperidol 5mg PO Q4H PRN o Other names: Haldol, Haldol Decanoate o Therapeutic Class: antipsychotics o Pharmacologic Class: butyrophenones o Indication: acute and chronic psychotic disorders including schizophrenia, manic states, psychoses. Patients with schizophrenia who require parenteral (IM) antipsychotic therapy o Why is this patient using this medication? For the agitation. o Mechanism of Action: alters the effects of dopamine in the CNS. Also has anticholinergic and blocking activity o Site of Metabolism: mostly metabolized the liver o Mechanism of Action: antagonizes the effects of histamine at H1 receptor does o o o o o o not bind to or inactivate histamine. Significant CNS depressant and anticholinergic properties Site of Metabolism: metabolized the liver hr Contraindications: hypersensitivity, acute attacks of asthmas, lactation Adverse Effects: drowsiness, dizziness, headache, blurred vision, tinnitus, hypotension, palpitations, anorexia, dry mouth, constipation, nausea, dysuria, frequency, urinary retention, photosensitivity, chest tightness, thickened bronchial secretions, wheezing, pain at IM site Nursing Assess movement disorder before and after administration. Avoid subcut injections. Required Lab Monitoring Frequency of Testing: May decreased skin response to allergy tests. Discontinue 4 days before skin testing. May cause dry mouth instruct patient to use frequent mouth rinses, good oral hygiene, and sugarless gum or candy to minimize this effect. May cause drowsiness caution patient to avoid driving or other activities requiring alertness until the response to drug is known. Caution patient to avoid use of alcohol and other CNS depressants concurrently with this medication. Advise patient to use sunscreen and protective clothing to prevent photosensitivity reactions. Trazodone 25 mg PO QHS PRN SEE ABOVE MEDICATIONS
Patient Research - Schizophrenia
Course: Nursing Practice Mental Health Nursing (Nurs 279)
University: MacEwan University

- Discover more from: