- Information
- AI Chat
Mental Health Final Study Guide
Nursing Concepts for Psychiatric/Mental Health Nursing (NUR 317)
Arizona State University
Recommended for you
Students also viewed
- Psychiatric Mental Health Nursing Success Chapter 1 Mental Health Mental Illness Theoretical Concepts
- Psychiatric Mental Health Nursing Success Chapter 1 Mental Health Mental Illness Theoretical Concepts
- Basic Concepts in Psychiatric Mental Health Nursing Study Guide Nclex Review Questions And Answers
- Mental Health Study Notes- week 8
- Mental Health 1 Study Notes
- 017 Exam 2 study guide Fall 2015 2
Related Studylists
physc term 3Preview text
ATI Mental Health Final Study Guide
Theories and Therapies
- Freud o Psychoanalysis: therapeutic process of assessing unconscious thoughts and feelings and resolving conflict ▪ Past relationships are the common focus ▪ Disadvantage: lengthy o Personality structure ▪ Id: pleasure principle and reflex action (think hungry newborn crying) ▪ Ego: problem solver and reality tester ▪ Superego: moral component of personality o Defense mechanisms and anxiety ▪ Operate at an unconscious level ▪ Defense mechanisms work by denying, falsifying, or distorting reality to make it less threatening o Experience during the early stages of life determines how you react ▪ Individuals’ lifetime adjustment patterns ▪ Personality traits o Transference vs countertransference
- Erikson o 8 stages of development ▪ Infancy (0-1 ½ yrs) – Trust vs mistrust ▪ Early Childhood (1 ½ - 3 yrs) – Autonomy vs shame and doubt ▪ Preschool (3-6 yrs) – Initiative vs guilt ▪ School-age (6-12 yrs) – Industry vs inferiority ▪ Adolescence (12-20 yrs) – Identity vs role confusion ▪ Early Adulthood (20-35 yrs) – Intimacy vs isolation ▪ Middle Adulthood (35-65 yrs) – Generativity vs self-absorption ▪ Later Years (65+ yrs) – Integrity vs despair o Development model, we use in the nursing assessment o Helps to determine what types of nursing interventions are most likely to be effective
- Sullivan o Foundation for Hildegard Peplau’s theory o The purpose of all your client’s behavior is to get their needs met through interpersonal interactionsand to reduce or avoid anxiety o Proposed that the nurse-client relationship “facilitates forward movement” for the nurse and the client o The process of nurse working with a client is to: ▪ Facilitate the client’s boundary management ▪ Independent problem solving ▪ Decision-making that promotes autonomy by modeling good behaviors and correcting bad behavior
- Hildegard Peplau o Art of nursing ▪ Provide care, compassion, and advocacy – enhance comfort and well-being o Science of Nursing
▪ Application of knowledge to understand a broad range of human problems and intervene in relieving patient suffering and promoting growth o *** Preorientation, orientation, working, termination phase o Determine the level of the client's anxiety provide interventions to lower anxiety aiming to improve thepatient’s ability to think and function o Peplau established the foundation for the professional practice of psychiatric nursing, she also continued to enrich psychiatric nursing theory and work for the advancement of nursing practice throughout her career
- Ellis o Rational-emotive behavior therapy ▪ Aims to eradicate irrational beliefs ▪ Recognize thoughts that are not accurate
- Beck o Cognitive-behavioral therapy ▪ Test distorted beliefs and change way of thinking; to reduce symptoms ▪ A most common type of therapy used by therapists ▪ Works under the premise that thoughts come before feelings and actions – therefore thetherapist works to change maladaptive thoughts ▪ Cognitive distortions: all-or-nothing thinking, over-generalization, labeling, mental filter, disqualifying the positive, jumping to conclusions, mind-reading, fortune-telling error, magnification or minimization, catastrophizing, emotional reasoning, “should” and “must” statements, personalization ▪ CBT challenges whether thought is based on reality, and provides a new thought- repetition of the new thought (actually builds new neuronal pathways in the brain)
- Maslow o Hierarchy of Needs ▪ Human beings are active participants in life, striving for self- actualization ▪ When lower needs are met, higher needs can emerge ▪ Emphasizes human potentialand the patient’s strength ▪ Prioritize nursing actions
- Prochaska: stages of changes a client is prepared to make o 5 steps – used in addiction
- Jellinek: a curve of progression from addiction/use to recovery
Varcarolis Chapter 3
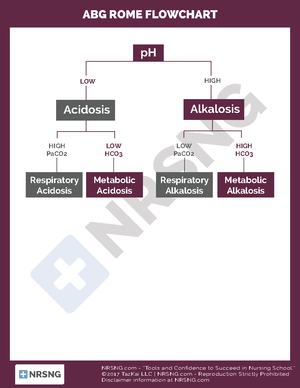
- Neurotransmitters o Schizophrenia – high dopamine o Depression – low serotonin/norepinephrine o Anxiety – low GABA, high glutamate o Mania – high serotonin/norepinephrine, high dopamine o Alzheimer's – low acetylcholine (ACH) o Parkinson’s – low dopamine, low acetylcholine
ATI Chapter 1
Psychosocial history o Perception of own health beliefs, illness, and wellness o Activity/leisure activities, how the client passes the time o Use of substances/substance use disorder o Stress level and coping abilities: usual coping strategies, support systems
Levels of Consciousness o Alert: client is responsive and able to fully respond by opening her eyes and attending to a the normal tone of voice and speech – answers questions spontaneously and appropriately o Lethargic: client can open her eyes and respond but is drowsy and falls asleep readily o Stuporous: the client requires vigorous or painful stimuli (pinching a tendon or rubbing the sternum) to elicit a brief response – might not be able to respond verbally o Comatose: client is unconscious and does not respond to painful stimuli ▪ Abnormal posturing of comatose client: - Decorticate rigidity: flexion and internal rotation of upper- extremity joints and legs - Decerebrate rigidity: neck and elbow extension, wrist and finger flexion
Assessing the client's memory o Immediate: ask the client to repeat a series of numbers or a list of objects o Recent: ask the client to recall recent events, such as visitors from the current day, or the purpose of the current mental health appointment or admission o Remote: ask the client to state a fact from his past that is verifiable, such as his birth date or his mother’s maiden name
Mini-mental status examination (MSE) o Used to objectively assess a client’s cognitive status by evaluating the following: ▪ Orientation to time and place ▪ Attention span and ability to calculate by counting backward by sevens ▪ Registration and recalling of objects ▪ Language, including naming of objects, following commands, and ability to write
Glasgow Coma Scale o Used to obtain baseline assessment of a client’s LOC, and for ongoing assessment o Eye, verbal, and motor response is evaluated, and a number value based on that response is assigned o The highest number possible is 15: which indicates the client is awake and responding appropriately o A score of less than 7 or less: indicates that the client is in a coma
Use the standardized assessment tool, Home environment, Education/employment, Activities, Drug and substance use, Sexuality and Suicide/depression, Savagery (HEADSSS) psychosocial assessment, to evaluate risk factors in the adolescents
Nurses use DSM-5 in the mental health setting to identify diagnoses and diagnostic criteria to guide assessment; to identify nursing diagnoses, and to plan, implement, and evaluate care
ATI Chapter 2
Ethical principles o Beneficence: the quality of doing good; can be described as charity o Autonomy: client’s right to make their own decisions, but the client must accept the consequences ofthose decisions – the client must also respect the decisions of others o Justice: fair and equal treatment for all o Fidelity: loyalty and faithfulness to the client and one’s duty o Veracity: honesty when dealing with a client
Types of admission o Voluntary admission: client or client’s guardian chooses admission to maintain treatment ***has the right to apply for release at any time – the client is considered competent, has the right torefuse meds and treatment o Temporary emergency admission: client is admitted due to the inability to make decisions regarding care – length varies by the client’s needs and state laws but often is not to exceed 15 days o Involuntary admission: client enters mental health facility against her will for an indefinite period – based on the client’s needs for psychiatric treatment, the risk of harm to self or others, or the inability to provide self-care ▪ Usually, 2 physicians are required to certify that the client’s condition requires commitment (varies from state to state) – which may be imposed by a family member, legal guardian, primary care provider, or a mental health provider ▪ The client can request a legal review of the admission at any time ▪ Limited to 60 days at which time a psychiatric and legal review of the admission is required ▪ The client still considered competent – has right to refuse meds and treatment ▪ If the client has been judged incompetent a temporary or permanent guardian will be appointed by the court to sign informed consent for the client. ***Guardian is expected to consider what the client would want if he were still competent o Long-term admission: similar to temporary commitment but must be imposed by the courts – time of commitment varies but typically 60-180 days, sometimes there is no set release date
The provider should prescribe seclusion and/or restraint for the shortest duration necessary and only if the least restrictive measures are not sufficient. They are for the physical protection of the client and/or the protection of other clients and staff
Rules for restraints o The provider must prescribe seclusion or restraint in writing o Time limits for seclusion or restraints are based on the age of the client: ▪ Age 18 or older: 4hr ▪ Age 9-17: 2hr ▪ Age 8 or younger: 1hr o The provider must reassess the client and rewrite the prescription, specifying the type of restraint every 24hr or the frequency of time specified by facility policy o Complete documentation every 15-30 minutes including a description of the following: ▪ Precipitating events and behaviors before seclusion/restraints ▪ Alternative actions are taken to avoid seclusion or restraint
Remind the client about the date of termination
Transference: occurs when the client views a member of the health care team as having characteristics of another person who has been significant to the client’s personal life o The client expects exclusive services from the nurse (e. extra session time) o The client demonstrates jealousy of the nurse’s time or attention o The client compares the nurse to a former authority figure
*** More likely to occur with a person of authority
- Countertransference: occurs when a health care team member displaces characteristics of people in her past onto a client o The nurse overly identifies with the client o The nurse competes with the client o The nurse argues with the client *** Clients who induce very strong personal feelings may become objects of countertransference
- Set up the following provisions to prevent client self-harm or harm by others o No access to sharp or otherwise harmful objects o Restriction of client access to restricted or locked areas o Monitoring of visitors o Restriction of alcohol and illegal substance access or use o Restriction of sexual activity among clients o Deterrence of elopement from the facility o Rapid de-escalation of disruptive and potentially violent behaviors through planned interventions by trained staff
Varcarolis Chapter 8
- Factors that promote patient growth – terms used in therapy o Genuineness: the key ingredient to building trust, patients know when you’re being fake o Empathy: we understand the patient's feeling, but we do not feel the patient feelings – not to be confusedwith sympathy o Positive regard: implies respect – viewing the other person as worthy of your care and can change – we show this in our attitudes and actions o Attending: a special kind of listening giving more intensity of presence, looking in the eyes, repeating what your hearing, make sure you understood by restating o Suspending value judgments: nurses are more effective when we guard against using our values to judge patient thoughts, feeling, or behaviors – suspending value judgment promotes patient disclosure and promotes healing o Helping patient develop resources: nurse learns the patient's strengths in situations that have occurredbefore and encourages patient toward modifying these actions for difficult situations
Varcarolis Chapter 9
- Use of silence: provides a meaningful time of reflection and time to weigh alternatives
- Clarifying techniques o Paraphrasing: restate in a different way o Restating: mirrors the exact message to allow for more info gathering
o Reflecting: assists patient to understand their feelings o Exploring: open-ended questions, “tell me more about...”
Communication techniques o Open-ended questions: encourage the patient to share information about experiences, perceptions or responses to a situation ▪ “What do you perceive as your biggest problem right now?” ▪ “What is an example of some of the stresses you are under right now?” ▪ “How would you describe your relationship with your wife?” o Close-ended questions: use sparingly, can give you specific and needed information – most useful during an initial assessment or intake interview or ascertain results ▪ “Are the medications helping you?” ▪ “When did you start hearing voices?” ▪ “Did you seek therapy after your first suicide attempt?” o Projective questions: start with “What if...” ▪ “If you had a wish for your family what would it be?” o Presupposition questions: miracle questions – helps them mourn what they are missing ▪ “Suppose you woke up this morning and this terrible accident didn’t happen; how would this have changed your life?”
Situations where you would be obligated to share information o Self-harm or intent to self-harm could mean suicide (always report to your clinical instructor) o Harm to others or intent to harm others – could be homicide o Child and elder abuse o NO MATTER WHAT – you are mandated by law to report abuse to the local authorities whether you believe it happened or not
Varcarolis Chapter 22
- Brains register pleasure by releasing dopamine in the nucleus accumbens
- Smoking or injecting drugs as opposed to swallowing a pill produces faster, stronger dopamine signal – more likely to lead to drug misuse
- Dopamine + glutamate = takeover of the brain’s reward system
- Repeated exposure to an addictive substance or behavior causes nerve cells in the nucleus accumbens to communicate with the prefrontal cortex that we no longer just want the drug, but we go after it
- Addictive drugs and behavior provide a shortcut, flooding the brain with dopamine o Can release 2-10 times the dopamine that natural rewards do – produce it faster and more reliably o Over time the brain releases less dopamine and no longer gives the same amount of pleasure
- User attempts more of the drug to obtain the same high because their brains have developed tolerance
- Addiction o Loss of control due to substance abuse or behavior o Use continues despite life problems o Tendency to relapse o Cravings continue (called conditioning) which increased the risk of relapse – triggers
- Risk factors for substance use o Genetic predisposition o Chronic stress – socioeconomic factors o Hx of trauma, abuse, combat experience
o 1 oz of whiskey or any other liquor
Males: 4 or more drinks a day and/or 14 or more in a week o Binge = 5 drinks at one time BAC 0.
Female: 3 or more drinks a day and/or 7 or more in a week o Binge = 4 drinks at one time BAC 0.
SAMHSA defines heavy alcohol use as binge drinking on 5 or more days in the past month
Common w/d symptoms: tremors, shakes, sweats, increased heart rate, increased blood pressure, N/V, muscle aches, seizures, fever
Alcohol withdrawal: can start just a few hours after decreasing use o Sxs peak after 48-72 hours then rapidly disappear unless the w/d progresses to alcohol w/d delirium o Watch for paradoxical w/d 5-7 days after initial detox – seizures
Alcohol w/d delirium o A medical emergency that can result in death o Best to provide one on one supervision o Usually require medical detox
Marijuana: THC is the active ingredient – that has depressant and hallucinogenic properties o Euphoria, detachment, relaxation – slowed perception of time, heightened sensitivity to eternal stimuli, sometimes anxiety, and paranoia o Long-term effects: lethargy, anhedonia, difficulty concentrating, loss of memory
Benzodiazepine o Sedation, disinhibition, decreased judgment, slurred speech, decreased coordination o Can cause falls in the elderly, paradoxical effect – DO NOT GIVE o Withdrawal: agitation, anxiety, panic, flushed feeling, increased HR, increased BP, diaphoresis, seizures, insomnia, pacing, extreme restlessness ▪ These can progress to seizures, confusion, and a loss of contact with reality
CNS Stimulants: cocaine, crack, amphetamines o Use symptoms: dilated pupils, dryness of the oronasal cavity (bleeding gums, nasal cavity, ulceration), excessive motor activity (jittery) o Withdrawal: depression and sleep o Cocaine takes effect in 4-6 seconds 5-7-minute-high follow then a deep depression ▪ Two main effects: anesthetic and stimulant ▪ Withdrawal symptoms: depression, paranoia, lethargy, anxiety, insomnia, N/V, sweating, chills
Opiates (oxycodone, hydrocodone, codeine, morphine, heroin, fentanyl) o Overdoses and deaths are often related to fentanyl derivatives being added o Effect: euphoria, marked sedation, confusion, constricted pupils, slowed breathing, intermittent consciousness, constipation, doctor shopping, shifting moods, financial issues o Watch for respiratory depression o Withdrawal: headache, N/V, diarrhea, muscles aches, sweating, fatigue, anxiety, insomnia, extreme craving
Synthetics o Ecstasy (MDMA) can cause serotonin syndrome if mixed with an SSRI o Use: euphoria, increased energy, increased self-confidence, increased sociability o Adverse effects: hyperthermia, heart failure, kidney failure, acute dehydration, serotonin syndrome
Dual diagnosis: suffering from mental illness and a comorbid substance abuse problem o Consider each a primary diagnosis and treatment at the same time
Denial and projection are commonly used
Medication-assisted therapy (MAT) *** gold standard for opioid addiction o Naltrexone, buprenorphine, or methadone combined with behavioral therapy o Suboxone (buprenorphine and naloxone) could at least double a person’s chances of remaining drug-free after 18 months o Buprenorphine reduces the number of overdose death, HIV from needle use, prostitution, and loss ofchildren to foster care o Naltrexone blocks opiate receptors and reduces or eliminates alcohol and opiate cravings ▪ Interfere with the mechanism of reinforcement o Disulfiram causes unpleasant physical effects ▪ Works on classical conditioning principle o Depakote, and Zyban – decrease cravings, only feel the bad effects, not the high of use o Methadone (Dolophine) ▪ Synthetic opiate blocks craving for and effects of heroin ▪ Only medication currently approved to treat the pregnant opioid addict o Clonidine (Catapres) ▪ Nonopioid suppressor of opioid withdrawal symptoms ▪ Effective somatic treatment when combined with naltrexone
Varcarolis Chapter 23
- Common causes of delirium o Infection/sepsis (UTI in the elderly) o Electrolyte imbalance - magnesium (1.5-2), potassium (3-5) o Substance use o Overmedication o Post-surgery o Impaired respiratory function – losing O o Stroke, fractures, vision loss
- Sundowners symptoms: rapid changes of mood, crying, anger, agitation, fear, pacing, stubbornness, depression, rocking, restlessness, inability to sleep
- 4 cardinal features of delirium o Acute onset and fluctuating course - may have hallucinations o Reduced ability to focus and/or sustain attention o Disorganized thinking o Disturbance of consciousness
- Dementia – has progressive deterioration o Long gradual decline in cognitive functioning over months to years o Difficulty with memory, judgment, executive functioning, can’t plan and problem solve o *** Advanced age is the biggest risk factor o Alzheimer’s disease o Lewy bodies (type of dementia affected by ABN protein in neurons) o Vascular- stroke o Traumatic brain injury o Alzheimer’s
o Perceived: any loss defined by the client that may not be obvious to others (loss of animal, loss of independence) o Actual: any loss of a valued person or item o Situational: unanticipated loss caused by an external event o Maturational: losses normally expected due to the developmental processing of life o *** treat all as actual losses
Kubler-Ross 5 Stages of Grief – may not experience stages in order, the length of each stage will varyfromperson to person o Denial o Anger o Bargaining o Depression o Acceptance
Bowlby 4 Stages of Grief – observed in client grieving (as young as 6yo) o Numbness or protest o Disequilibrium o Disorganization and despair o Reorganization
Engel 5 Stages of Grief o Shock and disbelief – numbness and denial o Developing awareness – begins within hours o Restitution – funeral o Resolution of the loss o Recovery
Worden 4 Tasks of Mourning o Task 1: accepting the reality of the loss o Task 2: processing the pain of grief – client uses coping mechanisms to deal with the emotional pain of the loss o Task 3: adjusting to a world without the lost entity – client changes the environment to accommodate the absence of the deceased o Task 4: finding an enduring connection with the lost entity in the mindset of embarking on a new life – client finds a way to keep the lost entity a part of her life while at the same time moving forward with life and establishing new relationships
Normal grief o Emotions include: anger, resentment, withdrawal, hopelessness, and guilt o Should achieve some acceptance by 6 months o Somatic symptoms: chest pain, palpitations, headaches, nausea, fatigue, sleep pattern issue
Anticipatory grief o Implies the “letting go” of an object or person before the loss, as in the case of a terminal illness o Individuals have the opportunity to grieve before the actual loss
Maladaptive grief o Delayed or inhibited grief o A distorted or exaggerated grief response o Chronic or prolonged grief ▪ The maladaptive response is difficult to identify due to the varying lengths of time requiredby clients to work through stages
▪ Clients remain in the denial stages of grief ▪ Chronic grief can result in the client’s inability to perform ADL
ATI Chapter 21 Medications for Anxiety and Trauma- and Stressor-Related Disorders
- Meds for anxiety o Benzodiazepine sedative hypnotic anxiolytics ▪ Lorazepam (Ativan), alprazolam (Xanax), clonazepam (Klonopin), diazepam (Valium) o Atypical anxiolytics/nonbarbiturate anxiolytics ▪ Buspirone o SSRI’s ▪ fluoxetine, citalopram, escitalopram (Lexapro), paroxetine, sertraline (Zoloft), Vilazodone o SNRI’s ▪ Venlafaxine, duloxetine, desvenlafaxine o Other antidepressants ▪ TCAs: amitriptyline, imipramine, clomipramine ▪ MAOIs: phenelzine ▪ Antihistamines: hydroxyzine pamoate, hydroxyzine hydrochloride ▪ Mirtazapine ▪ Trazodone o Betablockers: propranolol o Centrally acting alpha-blockers: prazosin o Anticonvulsant: gabapentin
ATI Chapter 22 Medications for Depressive Disorders
SSRI’s o Fluoxetine o Citalopram o Escitalopram o Paroxetine o Sertraline o Vilazodone
SNRI’s o Venlafaxine (Effexor) o Duloxetine (Cymbalta) o Desvenlafaxine o Levomilnacipran
Atypical antidepressants: inhibits dopamine reuptake – leaves more dopamine in the intracellular space o Bupropion
TCA’s o Amitriptyline o Imipramine o Doxepin o Nortriptyline o Amoxapine o Trimipramine
o Lorazepam
- Antidepressants o Buproprion o Venlafaxine o SSRIs
ATI Chapter 24 Medications for Psychotic Disorders
- First-generation o Chlorpromazine, low potency o Haloperidol, high potency o Fluphenazine, high potency o Loxapine, medium potency o Thioridazine, low potency o Thiothixene, high potency o Perphenazine, medium potency o Trifluoperazine, high potency
- Second-generation and third-generation (Atypicals) o Risperidone (Risperdal) o Quetiapine o Clozapine o Olanzapine o Lurasidone o Ziprasidone o Paliperidone o Iloperidone o Asenapine o Aripiprazole (Abilify) – 3 rd gen
ATI Chapter 26 Medications for Substance Use Disorders
- Opioid o Methadone substitution o Clonidine o Buprenorphine
- Alcohol o Withdrawal ▪ Benzodiazepines: chlordiazepoxide, diazepam, lorazepam, oxazepam ▪ Adjunct meds: carbamazepine, clonidine, propranolol, atenolol o Abstinence maintenance ▪ Disulfiram ▪ Naltrexone ▪ Acamprosate
- Nicotine o Bupropion o Nicotine replacement therapy o Varenicline
Mental Health Final Study Guide
Course: Nursing Concepts for Psychiatric/Mental Health Nursing (NUR 317)
University: Arizona State University

- Discover more from:
Recommended for you
Students also viewed
- Psychiatric Mental Health Nursing Success Chapter 1 Mental Health Mental Illness Theoretical Concepts
- Psychiatric Mental Health Nursing Success Chapter 1 Mental Health Mental Illness Theoretical Concepts
- Basic Concepts in Psychiatric Mental Health Nursing Study Guide Nclex Review Questions And Answers
- Mental Health Study Notes- week 8
- Mental Health 1 Study Notes
- 017 Exam 2 study guide Fall 2015 2