- Information
- AI Chat
Health Assessment Exam 3 Study Guide
Health Assessment (NSG 121)
Herzing University
Recommended for you
Preview text
Health Assessment Exam 3 Study Guide
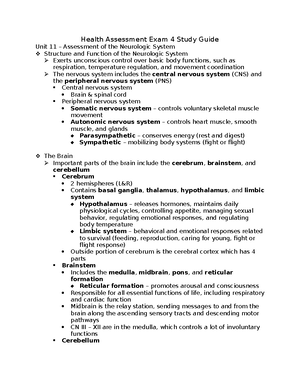
Unit 8 – Assessment of the Cardiovascular, Peripheral Vascular, and Lymphatic Systems Structure and Function of the CV System Assessment General appearance Inspection – skin color (blood flow to area), JVD, precordium, or edema in extremities When auscultating, listen for 1 full minute in each area Landmarks Pneumonic – APE to MAN Aortic area 2 nd intercostal space R of the sternal border Pulmonic area 2 nd intercostal space L of the sternal border Erb’s point 3 rd intercostal space L of the sternal border Where S2 is best heard Tricuspid area 4 th intercostal space L of the sternal border Mitral area 5 th intercostal space on the midclavicular line Point of maximal impulse – apex
Arteries and Veins of the Neck Carotid arteries – carry blood to the brain Jugular veins – used to assess fluid volume overload JVD = > 3 cm Carotid sounds Auscultate for bruits typically due to atherosclerosis changes
To assess a client’s jugular veins, the nurse will position the client supine with the head of the bed at 30-45 degrees Electrical Conduction Path The heart conduction system is a network of nodes, cells, and signals that control your heartbeat SA Node Fires at a rate of 60 – 100 bpm Is considered the pace maker of the heart The SA node’s electrical signals normally cause the atria of an adult’s heart to contract at a rate of about 60 to 100 times a minute Disturbance anywhere along this electrical pathway can cause irregular heartbeats (arrhythmia) AV Node Controls the ventricles The intrinsic rate of the AV node is 40 to 60 bpm Pathway SA Node AV Node Bundle Branches Purkinje Fibers
Structure and Functions of the PV and Lymphatic Systems Arterial blood flow regulation The arterial system is responsible for carrying oxygenated blood from the heart to the body It is a high-pressure system that is regulated by the pumping of the heart, muscle layer in the artery, and the internal elastic membrane Venous blood flow regulation
Frequent urination Leg pain Leg edema
Objective Data Collection – Neck and Vessel Exam Assessment techniques and positioning
Assessing for Cardiac Disease Check for fluid volume overload JVD, edema, weight gain, increase in need to urinate Decreased cardiac function SOB, fatigue with activity
Doppler VS Duplex Doppler Done at the bedside by an RN, no order needed Duplex Done by sonographer, needs an MD order
Heart Sounds and Representations S1 – lub Identifies onset of systole When AV valves close and ventricles contract S2 – dub Identifies the end of systole When AV valves open and ventricles fill with blood S Ventricles gallop occurs with fluid overload or HF Can be heard after S Sounds like lub-dub-dah This is an EARLY diastolic ventricular filling S Atrial gallop can occur with decreased ventricular compliance or CAD Occurs prior to S Sounds like ta-lub-dub Murmur Blowing or whooshing sound signifies turbulent blood flow typically due to a valvular defect Multiple types of murmurs dependent on area of disease Document murmurs to describe intensity, pitch, pattern, and location Pleural Friction Rubs Caused by inflammation of the pericardium Sounds like sandpaper being rubbed together Clicks
Associated with mitral valve prolapse
Stable VS Unstable Angina Stable angina Episodic Crescendo – decrescendo Occurs on exertion, relieved by rest Lasts 2-5 minutes Unstable angina Severe and of new onset Crescendo pattern Occurs at rest Lasts > 10 minutes
Peripheral Circulation Assessment of the lower extremities
Peripheral Pulse and Lymph Node Assessment
Cardiac Problems Intermittent claudication – symptoms of PAD causes pain during exertion and relieved with rest Deep vein thrombosis – unilateral acute pain, swelling, warmth, and erythema Note color Temperature – warmer than nonaffected limb Pulse Pain if pt flexes calf Measures width of calf to get a baseline measurement Chronic venous insufficiency – chronic dull and aching pain accompanied by edema Acute arterial occlusion – characterized by 7 P’s (pain, polar, paresthesia, paralysis, pallor, pulse, perfusion)
Artery Disease CAD – coronary artery disease Plaque buildup of the coronary arteries, those that supply blood to the myocardium Plaque can rupture or can occlude the lumen, leading to ischemia Ischemia = pain Inability to restore blood flow leads to cellular death PAD – peripheral artery disease Most common risk factors: Age, smoking, diabetes mellitus
Alteration in Sexual Function
Risk Factors for GI/GU Illness
Abdominal Assessment Techniques and Findings Guarding – voluntary contraction/tensing of abdominal wall due to pain or fear Rigidity – involuntary contraction due to peritoneal inflammation (reflex pt cannot control) Blumberg sign (rebound tenderness) – sign of inflammation/peritonitis Murphy sign Iliopsoas muscle test Ascites – abnormal fluid collection in the peritoneal cavity can be caused by liver disease r/t hepatitis, ETOH abuse, hepatotoxic medications, CHF CKD Assess using the wave test
Auscultation of the Abdomen Begin in the RLQ and move in a clockwise direction noting bowel sounds Hyperactive – > 35/min Hypoactive – < 5/min Absent 0 in 5 min Normoactive – 5-35/min
Palpation of the Abdomen Use the flat of the hand to detect palpable organs, abnormal masses or tenderness If pt reports pain, palpate that area LAST Light palpation – 1 cm deep Deep palpation is a technique used by advanced practice clinicians to assess for enlarged organs
Assessment of GU System Take note of: Dysuria Urinary frequency or urgency Urinary incontinence Difficulty starting flow of urine (prostate issue in men) Discharge from the vagina or penis Itching or odor Hx of STDs
Prostate Examination Tell the pt to urinate prior to the exam as palpation of prostate can press onto the bladder
Advanced technique done by an MD, not an RN
Papanicolaou Test (PAP Smear) A procedure to test for cervical cancer in women Advanced practice technique done by an MD Nurses can assist by: Gathering supplies and being a witness Gathering samples for culture during PAP and/or routine vaginal exam Telling pt to urinate prior to test Drape pt to expose genitals, but keep the legs partially covered Tell pt they may keep their socks on for comfort If pt is menstruating, must reschedule PAP
Male Genitourinary and GI Assessment Normal VS abnormal findings
Female Genitourinary and GI Assessment Findings
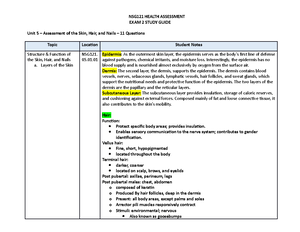
Unit 10 – Assessment of the Musculoskeletal system The Musculoskeletal System Composed of skeletal muscle and five types of connective tissues: bone, cartilage, ligaments, tendons, and fascia Muscles and bones facilitate movement through the joints or articulations
Structures in the Musculoskeletal System Meniscus Cartilage disk located between bones that absorb shock and cushion joints Cartilage allows bones to slide over one another to reduce friction Fascia Flat sheets that line and protect muscle fibers, attaching muscle to bone Ligaments Connect bone to bone to stabilize joints and limit movement
Functions of the Connective Tissue
Types of Joints Synovial (diarthrotic) joints – The most common type of joint
Rotation (internal, external, pronate, supinate) Circumduction – circular motion that combines flexion, extension, abduction, and adduction Inversion/eversion – moving the foot in and out Retraction Elevation/depression Opposition – moving the thumb to touch the little finger
Health Assessment Exam 3 Study Guide
Course: Health Assessment (NSG 121)
University: Herzing University

- Discover more from: