- Information
- AI Chat
Was this document helpful?
Shadow Health GI TIna Jones
Course: Diagnostic assessment (MSN610)
31 Documents
Students shared 31 documents in this course
University: Northern Kentucky University
Was this document helpful?

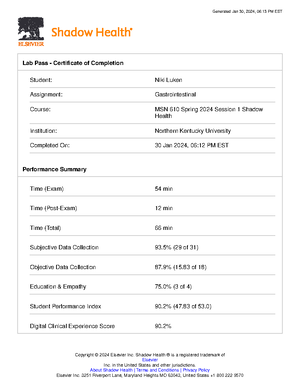
Gastrointestinal Results | Completed
MSN 610 Spring 2024 Session 1 Shadow Health, NUR
Return to Assignment (/assignments/920740/)
Subjective Data Collection: 31 of 31 (100.0%)
Chief Complaint
History of Present Illness
Your Results
Turn In (/assignment_attempts/16071140/choose)
Lab Pass (/assignment_attempts/16071140/lab_pass.pd
Overview
Transcript
Subjective Data Collection
Objective Data Collection
Education & Empathy
Documentation
Video Tutorial
Student Survey
Indicates an item that
you found.
Indicates an item that
is available to be found.
Category Scored Items
Experts selected these topics as essential
components of a strong, thorough interview with
this patient.
Patient Data
Not Scored
A combination of open and closed questions
yield better patient data. The following details
are facts of the patient's case.
Established chief complaint Reports frequently occurring stomach pain
Asked about onset of pain Reports noticing pain for "at least a month"
Reports that pain increased gradually
Asked about frequency of pain Reports pain occurs every day
Reports 3 to 4 episodes a week that are
more severe
Asked about duration of pain Pain begins right after finishing a meal
Hover To Reveal...
Hover over the
Patient Data
items
below to reveal important
information, including
Pro Tips
and
Example Questions
.