- Information
- AI Chat
This is a Premium Document. Some documents on Studocu are Premium. Upgrade to Premium to unlock it.
Was this document helpful?
This is a Premium Document. Some documents on Studocu are Premium. Upgrade to Premium to unlock it.
Mental Health SBAR Plan of Care
Course: Psychiatric-Mental Health Nursing of Individuals (NURS 3481)
100 Documents
Students shared 100 documents in this course
University: The University of Texas at Arlington
Was this document helpful?
This is a preview
Do you want full access? Go Premium and unlock all 4 pages
Access to all documents
Get Unlimited Downloads
Improve your grades
Already Premium?

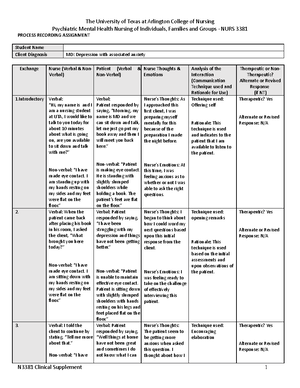
SBAR NURSING CARE PLAN
Student Name: Alexander Pham Client Initials: AA Age: 14- DOB: 01/23/2007
S:
Situation
Psychiatric Diagnoses: Major depressive
disorder with increased levels of anxiety
aggravated from environmental stressors.
Medical Problems: history of autism and
also experiences alcohol, nicotine, and
cannabis use disorder that adds on to the
patient’s physical symptoms of the
psychiatric diagnose.
Current issues (Chief Complaint, Precipitating Factors)
The chief complaint was described as having suicidal
ideations as evidenced by holding a knife close to the
abdomen for two minutes but did not follow through with
puncturing through the skin. The girlfriend was the person
who made the call for the police to show up when he was
experiencing this episode.
B:
Background
Psychosocial/Environmental History (Predisposing Factors): Family history of mental illness but states, “I
do not know exactly what they are called but they are related to drug abuse.”
Neurological / Genetic History (Predisposing Factors): The client stated that the environmental factors of
living situation, family relationships, and availability of substances subject to abuse, are predisposing
factors to the diagnoses. Patient states, “I started drinking alcohol when I was 12, then smoked cigarettes
and cannabis when I was about 14.”
A:
Assessment
Mental Status Assessment
Appearance: Dress is appropriate for age, red hair that is messy but grooming overall adequate for
situation.
Behavior: Able to maintain eye contact with normal mannerisms, body is erect with no signs of
slumping of the shoulders.
Speech: Normal volume and rate of speech that is clear and with precise tone.
Mood: Normal mood at the moment that question was asked but patient stated feelings of
worthlessness two days ago as evidenced by stating, “I sometimes don’t have the energy that I was had
before.”
Affect: No negative emotions or mood noted, client was cooperative and able to answer questions in a
professional manner.
Cognition: “alert and oriented x 4-, short- and long-term memory appropriate, abstract ability present.
Thought Process: clear, consistent and linear. No flight of ideas when not under the influence, the client
confirms this by saying that “I need to maintain and really take my sobriety serious if I want to actually
feel better.”
Thought Content: Patient’s thought content is consistent with the context of conversation. No thoughts
of suicidal or homicidal ideations at the time question was asked, the client does place blame on himself
many times by restating that, “the reason that I am here was because I wanted to commit suicide.”
Perceptual Disturbances: Patients reports no perceptual audible or visual disturbances.
Insight/Judgment: Good insight and judgement but dependent on willingness to maintain the current
level of sobriety.
Suicide ideation: Patients reports history of suicidal ideation as reason for admission. Reports no current
suicidal ideation. Prior SI included the plan of inflicting physical harm first through the head smashing
with various objects, then followed by puncturing the abdominal wall with a knife.
Homicide ideation: No homicidal ideation; patient denies having HI
Aggression: precautions placed for increased levels of aggression related to physical symptoms of
depression and increased levels of anxiety aggravated by certain stressors.
Psychosis: No evidence of psychosis noted.
Falls: Patient reports no issues with falls. Staff have no noted fall risk measure implemented.
Substance use: the client is a chronic alcohol, nicotine, and cannabis user due to availability and
environment within the household in which he grew up, this knowledge and accessibility is one of the
1
Why is this page out of focus?
This is a Premium document. Become Premium to read the whole document.