- Information
- AI Chat
Was this document helpful?
Mental Health Shadowhealth Tina Jones Documentation
Course: Family Nurse Practitioner Ii (NUR 535)
24 Documents
Students shared 24 documents in this course
University: Southern Connecticut State University
Was this document helpful?

1/3
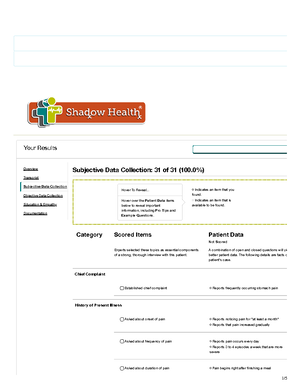
Mental Health Results | Turned In
Documentation / Electronic Health Record
Document: Provider Notes
Student Documentation Model Documentation
Your Results
Overview
Transcript
Subjective Data Collection
Objective Data Collection
Education & Empathy
Documentation
Document: Provider Notes
Students also viewed
- Focused Exam-Chest Pain Brian Foster Shadowhealth Objective
- Cardiovascular Shadowhealth Tina Jones Objective
- Focused Exam-Abdominal Pain Esther Parks Shadowhealth Objective
- Focused Exam-Cough Danny Rivera Shadowhealth Objective
- Shadow Health Gastrointestinal Tina Jones Documentation
- Tina Jones Shadowhealth Mental Health Subjective
Related documents
- Focused Exam-Cough Danny Rivera Shadowhealth Documentation
- Respiratory Shadowhealth Tina Jones Objective
- Focused Exam-Chest Pain Brian Foster Shadowhealth Documentation
- Focused Exam-Abdominal Pain Esther Parks Shadowhealth Documentation
- Heent Shadowhealth Tina Jones Documentation
- Focused Exam-Cough Danny Rivera Shadowhealth Subjective