- Information
- AI Chat
Shadow Health Gastrointestinal Tina Jones Documentation
Family Nurse Practitioner Ii (NUR 535)
Southern Connecticut State University
Recommended for you
Students also viewed
- Heent Shadowhealth Tina Jones Objective Data
- Focused Exam-Chest Pain Brian Foster Shadowhealth Objective
- Shadow Health Gastrointestinal Tina Jones Objective Assessment
- Heent Shadowhealth Tina Jones Subjective
- Gastrointestinal Tina Jones Subjective Shadowhealth
- Respiratory Shadowhealth Tina Jones Documentation
Related documents
Preview text
1/
Gastrointestinal Results | Turned In
Documentation / Electronic Health Record
Document: Provider Notes
Student Documentation Model Documentation
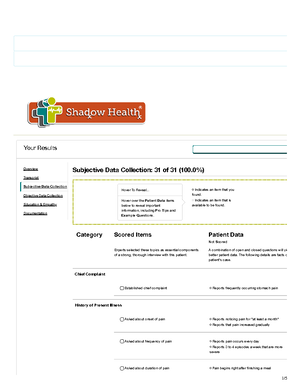
Your Results
Overview
Transcript
Subjective Data Collection
Objective Data Collection
Education & Empathy
Documentation
Document: Provider Notes
2/
Student Documentation Model Documentation
HPI: Ms. Jones is a pleasant 28-year-old African American wom who presented to the clinic with complaints of upper stomach after eating. She noticed the pain about a month ago. She stat that she experiences pain daily, but notes it to be worse 3-4 tim per week. Pain is a 5/10 and is located in her upper stomach. S describes it <kind of like heartburn= but states that it can be sh She notes it to increase with consumption of food and speciûc fast food and spicy food make pain worse. She does notice tha has increased burping after meals. She states that time genera makes the pain better, but notes that she does treat the pain <e few days= with an over the counter antacid with some relief.
Social History: She denies any speciûc changes in her diet rece but notes that she has increased her water intake. Breakfast is usually a muffin or pumpkin bread, lunch is a sandwich with ch dinner is a homemade meal of a meat and vegetable, snacks a French fries or pretzels. She denies coffee intake, but does drin cola on a regular basis. She denies use of tobacco and illicit dr She drinks alcohol occasionally, last was 2 weeks ago, and wa drink. She does not exercise.
Review of Systems: General: Denies changes in weight and ge fatigue. She denies fevers, chills, and night sweats. • Cardiac: D a diagnosis of hypertension, but states that she has been told blood pressure was high in the past. She denies known history murmurs, dyspnea on exertion, orthopnea, paroxysmal nocturn dyspnea, or edema.
- Respiratory: She denies shortness of breath, wheezing, cough sputum, hemoptysis, pneumonia, bronchitis, emphysema, tuberculosis. She has a history of asthma, last hospitalization w age 16, last chest XR was age 16. • Gastrointestinal: States tha general her appetite is unchanged, although she does note tha will occasionally experience loss of appetite in anticipation of t pain associated with eating. Denies nausea, vomiting, diarrhea constipation. Bowel movements are daily and generally brown color. Denies any change in stool color, consistency, or frequen Denies blood in stool, dark stools, or maroon stools. No blood emesis. No known jaundice, problems with liver or spleen.
General: Ms. Jones is a pleasant, obese 28-year-old African American woman in no acute distress. She is alert and oriented maintains eye contact throughout interview and examination.
- Abdominal: Abdomen is soft and protuberant without scars o lesions; skin is warm and dry, without tenting. Bowel sounds pr and normoactive in all quadrants. No tenderness to light or dee palpation. Tympanic throughout. Liver is 7 cm at the MCL and below the right costal margin. Spleen and bilateral kidneys are palpable. No CVA tenderness.
- Cardiovascular: Regular rate and rhythm, S1 and S2 present, murmurs, rubs, gallops, clicks, precordial movements. No bruit auscultation over abdominal aorta. No femoral, iliac, or renal br
- Respiratory: Chest is symmetrical with respirations. Lung sou clear to auscultation anteriorly and posteriorly without wheezes crackles, or cough.
Gastroesophageal reüux disease without evidence of esophagi
Shadow Health Gastrointestinal Tina Jones Documentation
Course: Family Nurse Practitioner Ii (NUR 535)
University: Southern Connecticut State University

Recommended for you
Students also viewed
- Heent Shadowhealth Tina Jones Objective Data
- Focused Exam-Chest Pain Brian Foster Shadowhealth Objective
- Shadow Health Gastrointestinal Tina Jones Objective Assessment
- Heent Shadowhealth Tina Jones Subjective
- Gastrointestinal Tina Jones Subjective Shadowhealth
- Respiratory Shadowhealth Tina Jones Documentation