- Information
- AI Chat
This is a Premium Document. Some documents on Studocu are Premium. Upgrade to Premium to unlock it.
Was this document helpful?
This is a Premium Document. Some documents on Studocu are Premium. Upgrade to Premium to unlock it.
Week4 DCE Tina Jones Comprehensive
Course: Advanced Health Assessment (NURS 6512)
554 Documents
Students shared 554 documents in this course
University: Walden University
Was this document helpful?
This is a preview
Do you want full access? Go Premium and unlock all 4 pages
Access to all documents
Get Unlimited Downloads
Improve your grades
Already Premium?

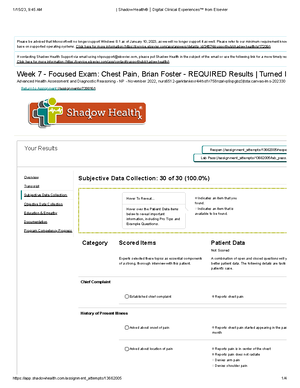
Documentation / Electronic Health Record
Document: Provider Notes
Document: Provider Notes
Student Documentation Model Documentation
Identifying Data & Reliability
Tina Jones is 28-year-old obese African American
female. Pleasant and cooperative. Present to the clinic
with recent right foot injury. Speech is clear and
coherent. Eye contact throughout the interview.
N/A
General Survey
Ms. Jones is well nourished and well developed,
appropriately dressed with good hygiene: Not in acute
distress.
N/A
Chief Complaint
"I scraped my foot a week ago and the wound is not
healing. And the pain is getting worse."
N/A
History Of Present Illness
Ms. Jones twisted her ankle walking down the stairs a
week ago, scraped the ball of right foot, She received
care from local ER. XRay of the foot and wound care
were provided in the ED. She was sent home with PRN
tramadol for pain and Neosporin topical agent for
wound. Right foot become red and swollen. C/O sharp
and throbbing pain at right foot. Pain was 7/10, two
hours after taking tramadol. Weight bearing as
aggravating factor and tramadol as relieving factors.
Reported of difficulty ambulating due to pain. she
reported of fever 102 last night.
N/A
Medications N/A
Why is this page out of focus?
This is a Premium document. Become Premium to read the whole document.